Uncategorized
Mechanical Ventilator
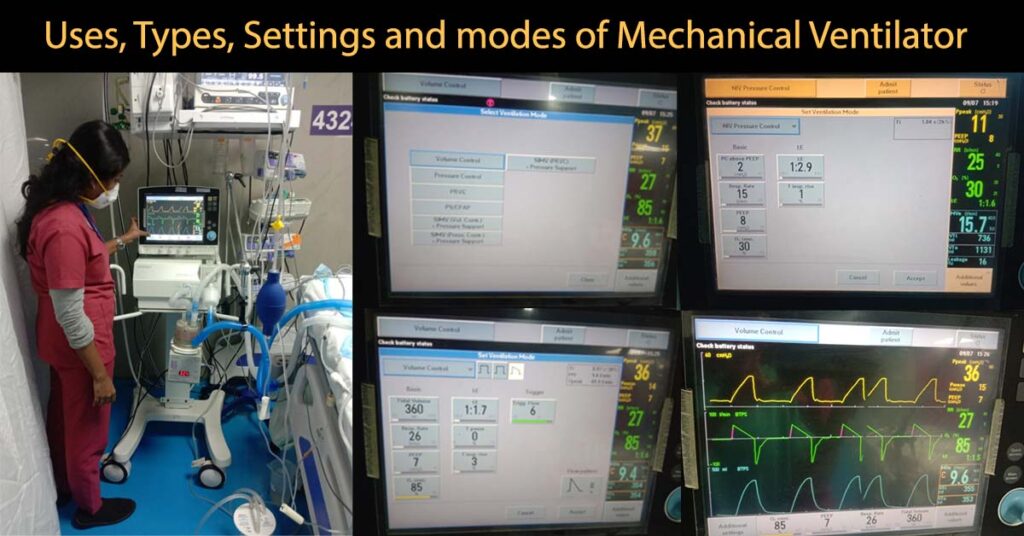
What is a Mechanical ventilator?
A mechanical ventilator is a machine, which provides artificial ventilation when the patient’s normal ventilation mechanism fails (Gives artificial breath when patient finds it difficult to breathe or unable to breathe on their own).
Ventilator provides oxygen and removes excess carbon dioxide (it acts as another lung).
Indication for mechanical ventilation: (When to start mechanical ventilation?)
- Acute hypoxemic (decreased oxygen levels in blood) respiratory failure
- Hypoventilation (breathes very slowly or very shallowly)
- Increased work of breathing
- Hemodynamic instability (abnormal body mechanisms due to disease condition)
- Cardio respiratory arrest (sudden loss of heart function)
- Flail chest (a part of rib cage is separated from rest of the chest wall due to severe trauma)
- Raised intracranial pressure (increased pressure inside the skull)
- Refractory shock (heart failure causes sudden drop in blood flow)
- Diseases like myasthenia gravis, motor neuron disease, guillain-barre syndrome
- Spinal cord injury
- Effect of drugs, anesthesia
What are the types of mechanical ventilation?
Ventilators are of 4 basic types.
- Negative pressure ventilator: Here a container encloses the whole body except the head (Iron Lung). Sucking out air from the container creates a negative pressure forcing the lung to expand, pulling air in to the lung.
- Pressure cycled ventilator: Air is pushed in to the lung in a preset pressure which follows passive expiration.
- Volume cycled ventilator: This type is the most commonly used. The ventilator delivers a preset volume of air and stops to allow passive expiration.
- High frequency ventilator: Here high respiratory rate with small tidal volume is used to keep the alveoli ventilated. Small tidal volume reduces barotraumas and cardiovascular damages.
Mechanical ventilators can be Invasive or Non Invasive
What is invasive ventilation?
In invasive ventilation air/oxygen is delivered through a tube placed inside the windpipe (Endo-tracheal intubation) or through Tracheostomy.
What is non-invasive ventilation?
In Non-invasive ventilation air or oxygen is delivered via a face mask avoiding endo-tracheal intubation.
What are ventilator settings?
Basic display orders in ventilator settings:
- Fio2 ( fraction of inspired oxygen )
Amount of oxygen present in the inspired air.
Normal range (21%-100%).
- Respiratory Rate ( RR )
complete one count of inspiration and expiration for one minute ( breathing rate ).
Respiratory rate is different for adults and neonates (newborns).
Normal Range of RR for adult: 12 – 16 breaths/minutes
Normal Range of RR for neonates: 40-60 breaths/minutes
- Tidal volume ( VT )
Volume of air present during normal inspiration and expiration.
Normal range: 4 – 8 ml per kg body weight (approximately 500ml)
- PEEP ( positive end expiratory pressure )
Pressure in the alveoli at the end of expiration. It prevents alveoli collapse.
Normal range: 5cmH2o – 10cmH2o.
What are the modes of ventilation? and What are the uses of the modes?
- Continuous mandatory ventilation (CMC).
- Assist – control ventilation (ACV).
- Intermittent mandatory ventilation (IMV).
- Synchronize intermittent mandatory ventilation (SIMV).
- Pressure support ventilation (PSV).
- Continuous positive pressure ventilation (CPAP).
- Bi-level positive pressure ventilation (BIPAP).
- Continuous Mandatory Ventilation (CMV): This mode delivers a preset tidal volume at a preset rate.CMV prevents patient to breathe on his own.
- Assist control ventilation: This mode is used in patients with normal respiratory drive with weak respiratory muscles. The machine assists the patient’s effort and provides ventilation according to the patient’s need.
- Intermittent Mandatory Ventilation: In IMV patient can initiate breathe between mandatory ventilations and the machine will deliver oxygenated air to support the breath.
- Synchronize intermittent mandatory ventilation (SIMV) synchronizes machine induced breaths with patient’s spontaneous breath. If the patient could not breathe within the preset time the device delivers a mandatory breath.
- Pressure support Ventilation: Here the machine delivers positive pressure when the patient takes a breath of his own. The patient determines the rate.
- Continuous positive pressure ventilation (CPAP) Provides continuous positive pressure to the upper airway, to keep the airway open and prevent airway and alveoli collapse.
- Bi-level positive pressure ventilation (Bi-PAP) As CPAP, Bi-PAP provides positive pressure ventilation but it delivers different pressures (bi-level) during inhalation and exhalation. Inhalation pressure is between 8 to 10 cms of water and Exhalation pressure is between 2 to 4 Cms of water. Both CPAP and BIPAP are called as Non Invasive Ventilators.
What is weaning?
Weaning is the gradual withdrawal of ventilator support. Weaning is started when the cause is treated successfully.
What are the complications of Mechanical Ventilation?
The common complications of mechanical ventilation are: airway trauma, airway malfunction, acid base disturbances, oxygen toxicity, arrhythmias, barotraumas, infection, pneumothorax etc.
Mechanical Ventilator Read More »
What is Capnography?, Indications, Uses and Interpretations.
What is Capnography?
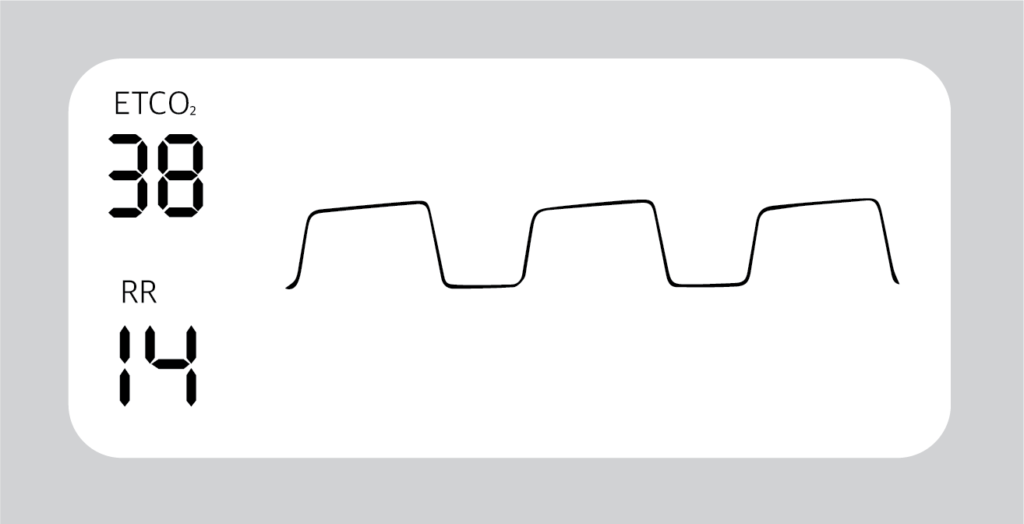
Capnography is a clinical procedure used for the measurement of CO2 levels in respired air at the end of expiration (End tidal CO2). In Capnography the results are displayed in graphic and numerical form.
Graphic form gives more details to diagnose and assess the ventilation of the patient.
What is Capnometry?
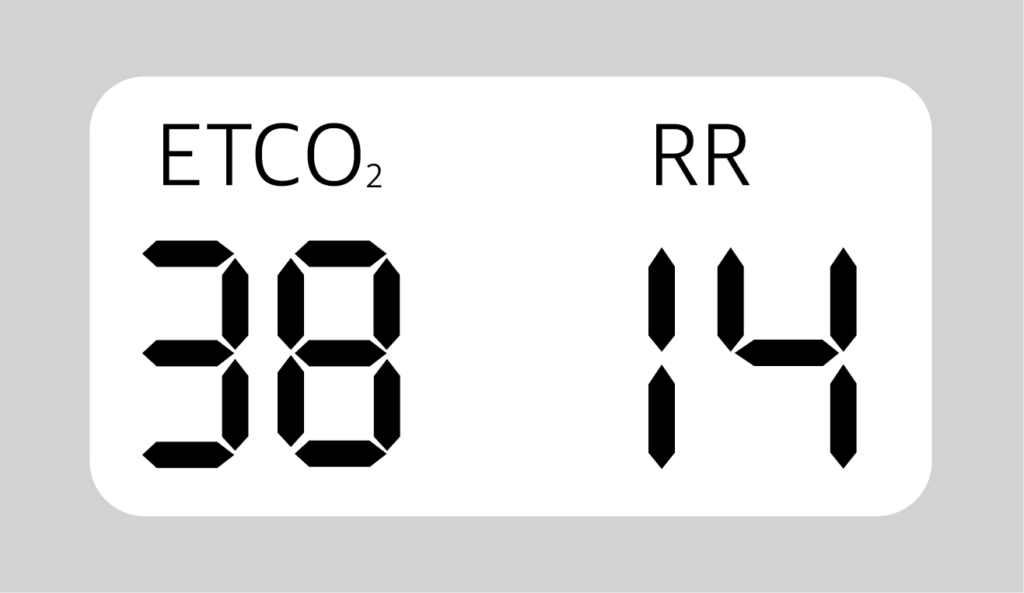
Capnometry is also used to measure End Tidal CO2 but gives results only in numerical form. (only in numbers and no graphic form)
How Capnography Works?
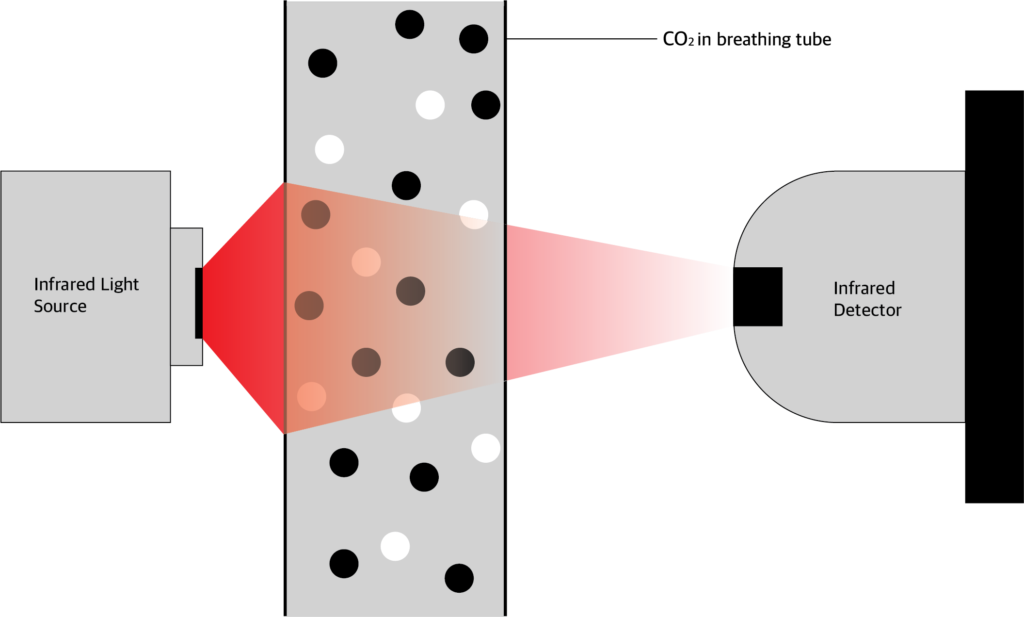
Carbon dioxide absorbs infrared light energy. The amount of infrared light absorbed depends on the CO2 concentration. In ccapnography device, CO2 is allowed to pass through infrared light.
The amount of light absorbed is calculated by comparing the amount of infrared light send from the source and the amount received by the photo detector.
From this the CO2 pressure is calculated and values given in graphic and numerical form.
What is the normal ETCO2 values?
Normal ETCO2 value is between 35 to 45 mmHg.
Normal respiratory rate is 14/min.
What are the indications of Capnography?
- Verification of artificial airway placement (intubated paient)
- Assessment of pulmonary circulation and respiratory status
- Assess V/Q relationship
- assess dead space and tidal volume ratio
- Optimization of mechanical ventilation
- Monitoring carbon dioxide elimination
- Screening patients for pulmonary embolism
- Assess the efficiency of ventilator support (PaCO2 – PETCO2)
What are the contraindications of capnography?
- There are no absolute contraindications to capnography in mechanical ventilator parients.
What are the types of Capnography?
- Mainstream
- Side stream
Mainstream
The mainstream analysier chamber placed between the endotracheal tube and the ventilator circuit.
Advantages:
- Sensor placed in breathin circuit.
- Fast response(crisp waveform)
- Short lag time
- No sample of gas removed to reduce tidal volume
Disadvantages:
- Required frequent calibration
- Secretions and humidity can block sensor’s window
- Difficult to use in non intubated patient
- Bulky sensor in airway
- Reusable adaptors require cleaning and sterilization
Side Stream
The side stream sensor is placed in the main unit and not in the airway. CO2 is aspirated through a sampling tube, connected to a T piece adapter.
Advantages:
- No bulk sensor or heater in the breathing circuit
- Disposable sampling line
- Ability to use with non intubated patient
Disadvantage:
- Secretions can block sampling tube
- Sample flow may decrease the tidal volume
- Lag time between CO2 change and measurement
- Slow response to CO2 change
- Frequent calibration is required
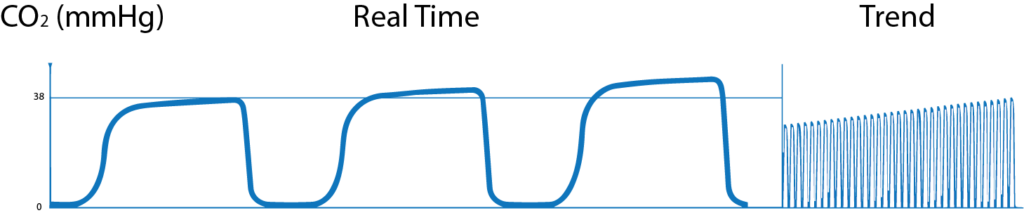
How to interpret the waves of Capnography?
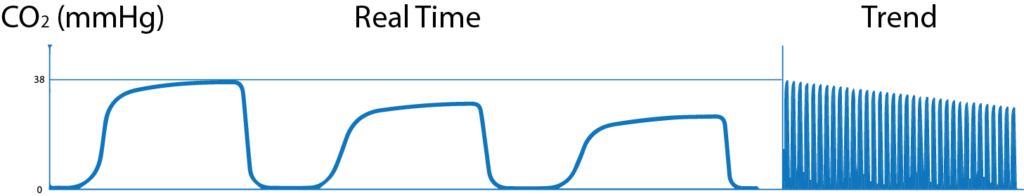
Normal Capnogram:

A-B: CO2 level is 0 mmHg. This shows the CO2 free air from dead space (Both anatomical and apparatus dead space)
B-C: In this phase, alveolar gas mixes with dead space gas, so there is steep increase in expired PCO2.
C-D: this phase is called Alveolar Plateau. Here as the CO2 rich gas is exhaled the alveoli becomes smaller and the concentration of CO2 increases towards
D: End of expiration showing End Tidal CO2.
D-E: in this phase inspiration starts and fresh CO2 free air is inhaled and so the PCO2 falls to 0.
Trend Graph: Shows changes in one hour.
Abnormal Capnogram:
1. Gradual increase in ETCO2
- Hypoventilation (Decreased Respiratory rate) and decreased tidal volume.,
- Increased metabolic rate, increased muscular activity,
- Malignant Hyperthermia (sudden raise in temperature)
- Good response to bronchodilators.
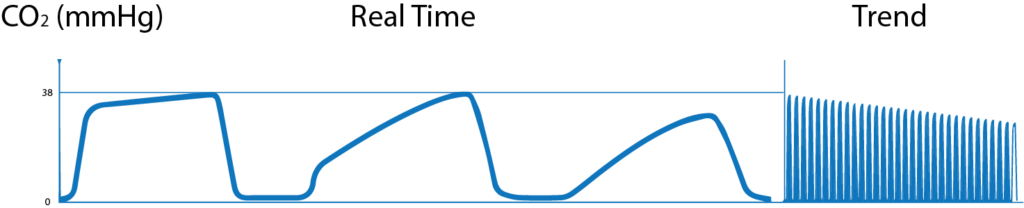
2. Gradual decrease in ETCO2
- Hyperventilation (increased respiratory rate) and increased tidal volume,
- Decreased metabolic rate, decreased muscular activity,
- Hypothermia (drop in temperature),
- Pulmonary embolism.
3. Airway obstruction
- Obstruction in breathing circuit,
- Foreign body in patient’s upper airway,
- Blocked or kinked artificial airway,
- Bronchospasm,
4. Cleft in wave
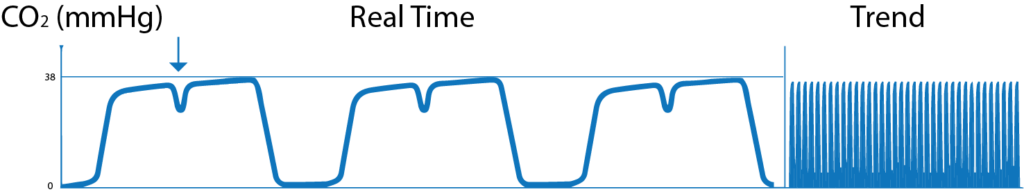
- When the action of the muscle relaxant, given to the patients subsides and when spontaneous breathing starts, cleft appears in plateau of the wave.
5. Transient wave form
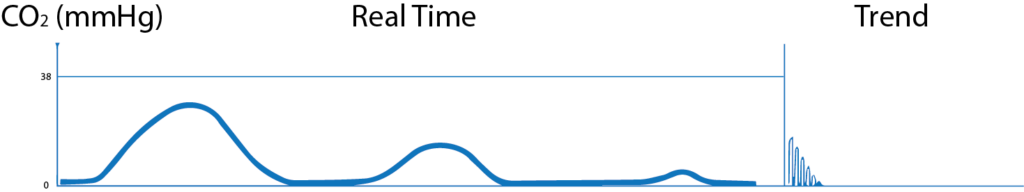
- When the endotracheal tube is in the oesophagus, no CO2 waves are seen or small transient waves are seen.
6. Distorted downward slope
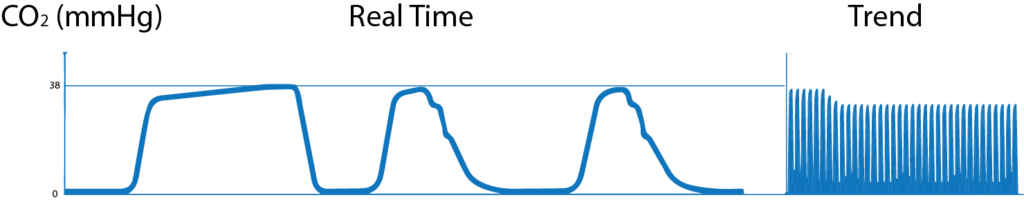
- Deflated or leaking tracheotomy or endotracheal tube and small artificial airway can produce distorted downward wave.
7. Base line elevated and abnormal descending limb

- Fault in exhalation valve of the ventilator
- Patient re breathing exhaled air can produce waves with base line elevation and abnormal descending limb.
8. Elevation of base line with corresponding increase in ETCO2

- Faulty expiratory valve
- Partial rebreathing
- Insufficient expiratory time
- Malfunction of CO2 absorber system
What is Capnography?, Indications, Uses and Interpretations. Read More »
Meconium Aspiration Syndrome
What is Mecomium Aspiration Syndrome?
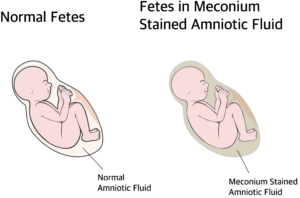
Meconium aspiration syndrome is a type of respiratory distress occurring in babies born with meconium stained amniotic fluid or aspirated meconium during delivery.
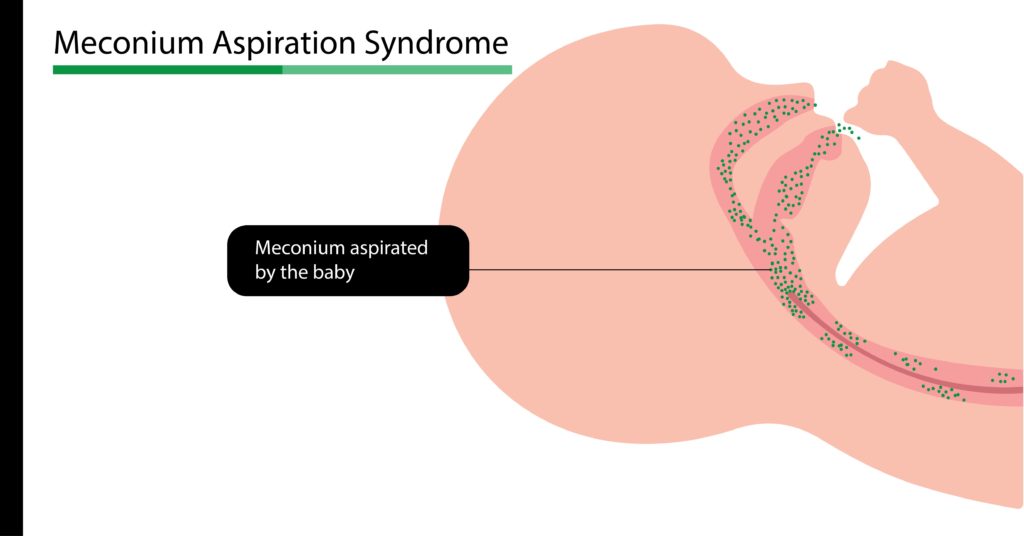
What is Meconium and how it is aspirated?
The term meconium refers to the sterile stool present in the fetal intestine. (earliest stool of the baby). Meconium contains epithelial cells of the intestine, lanugo (fetal hair), blood cells, bile, mucus, intestinal secretions and amniotic fluid. Meconium is thick, sticky, odorless and dark yellow to olive green in colour. Normally the child passes meconium hours after birth.
Passage of meconium is prevented by a low motilin level in the fetus. Motilin is a hormone (chemical) which controls motility of the intestine (peristalsis). Before delivery the motilin level will be low, preventing intestinal movements. Motilin is produced around 34 weeks of gestation. In full term and post dated babies the motilin level is high and when there is vagal stimulation by head or cord compression or stress inside uterus (hypoxia, acidosis etc) peristalsis increases and the anal sphincter is relaxed allowing meconium to come out.
This may occur during or before the delivery. Since the fetus is surrounded by the meconium stained amniotic fluid, when the baby gasps, it is aspirated into the lungs, resulting in Meconium Aspiration Syndrome.
Even though it’s sterile, it causes inflammation and may mechanically obstruct the airway, inactivate surfactant, and prevent gas exchange. Meconium aspiration syndrome is commonly found in full-term (>39 weeks) or post dated deliveries.
Depending upon the amount and duration of aspiration, the newborn may show symptoms ranging from mild to life-threatening distress. Therefore treatment has to be started as soon as possible.
What are the predisposing factors of MAS?
Mother’s:
- Post-term pregnancy
- Prolonged, hard delivery
- Hypertension, diabetes, preeclampsia
- Mother smoking during pregnancy and maternal drug abuse.
Fetal:
- Infection or stress to the fetus
- Decreased oxygen supply
- Cord or head compression.
What are the clinical features of Meconium Aspiration Syndrome?
- Newborn may have yellow discoloration of the umbilical cord, nail bed and skin
- Increased respiratory rate and difficulty in breathing
- May use extra muscle for breathing normally
- May have grunting and nasal flaring
- The newborn may have bluish discoloration of lips, hands, and legs
- The newborn may also have box-shaped (barrel-shaped) chest
- Chest sound through auscultation reveals rales and ronchi,
- Meconium stain on body
- May show signs of post maturity like peeling skin and long finger nails.
Other diseases with similar clinical signs (differential diagnosis):
- Respiratory Distress syndrome
- Perinatal asphyxia
- Transient Tachypnea of the New Born
- Congenital Heart Disease
- Surfactant deficiency
- Pneumonia and sepsis of newborn
What are the tests done in Meconium Aspiration Syndrome?
X-ray chest
- Irregular, linear, streaky infiltrates.
- Hyper inflated lungs,
- Flat diaphragm.
Pulseoxymeter
To measure oxygen saturation and degree of shunting
The blood flow of the heart in the fetus is different from that of the newborn. There will be a flow of blood directly to the left side bypassing the pulmonary circulation due to high pulmonary pressure. But this becomes normal when the pulmonary pressure drops as the baby takes the first breath.
When this process is interrupted, the pressure remains high and may result in Persistent Pulmonary hypertension of Neonates. Due to this, there will be always a difference of at least 10 % SpO2 between right hand (higher than other) and other limbs.
Arterial blood gas analysis
Decreased oxygen and increased CO2, acidosis. Echocardiogram and ECG to rule out heart diseases.
Blood and aspirated meconium for culture and drug sensitivity testing.
How Meconium Aspiration Syndrome baby is managed?
As soon as the head is delivered, suction is applied to mouth, nose and pharynx. Soon after the delivery the baby’s vitals assessed.
If the baby is vigorous (active)
Heart rate above 100/minute, having spontaneous breathing, spontaneous movements and good tone provide supportive care with frequent monitoring. No tracheal suctioning or intubation necessary.
If the baby is not vigorous (limp)
Baby having cyanosis, increased respiratory rate, reduced heart rate and the baby is limp without spontaneous breathing, tracheal suctioning is done.
Neonatal intensive care given.
Oxygen therapy using simple oxy hood (transparent helmet-like hood) or Continuous Positive Airway Pressure (CPAP) through a mask, ECMO (Extracorporeal membrane oxygenation) or Mechanical ventilation can be started according to the severity of distress.
Empirical antibiotics to prevent infection
Nitric oxide inhalation to open blood vessels and prevent pulmonary hypertension.
Surfactant replacement therapy to replace the inactivated surfactant and open alveoli. Chest physiotherapy.
How to prevent Meconium aspiration Syndrome?
- Good antenatal, ante partum and intra partum care can prevent MAS.
- Mothers should avoid smoking and drug abuse.
- Avoid post dated delivery by induced labor.
- Suctioning the nose, mouth and pharynx before the delivery of shoulders
- If the amniotic fluid is stained with meconium, the amniotic fluid can be diluted by infusing isotonic liquid in to the uterus (Amnioinfusion).
Meconium Aspiration Syndrome Read More »
Respiratory Distress Syndrome (RDS) in Neonates

What is Respiratory Distress Syndrome (RDS) in Neonates?
RDS once called Hyaline Membrane Disease (HMD) or Surfactant deficiency syndrome (SDD) is mainly seen in premature babies and manifest within few hours of birth due to surfactant deficiency and immature lungs. May cause death due to respiratory distress or insufficiency, if not treated on time.
What are the causes of Respiratory Distress Syndrome?
The main causes are immature development of the lung and inadequate surfactant (adequate surfactant, prevents collapse of the alveoli by reducing the surface tension of the fluid lining of the alveoli).
What are the most common contributing factors?
- Early birth (born before 7 months of pregnancy)
- When the mother has Diabetes mellitus
- When the newborn is born through Cesarean section delivery
- The previous sibling had RDS
- Hypothermia of the newborn
Pathophysiology of RDS
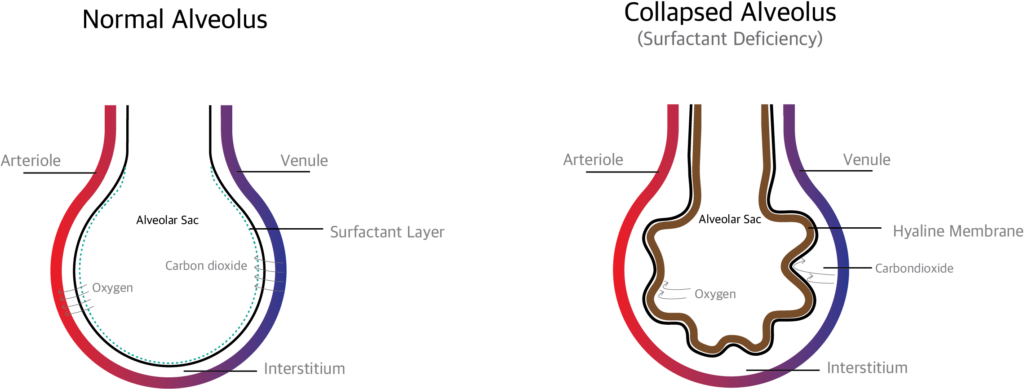
The surfactant production starts by 24 weeks of pregnancy. In case the baby is born before this period, there is a higher chance of surfactant deficiency which leads to respiratory distress.
Normally when the baby is in mother’s uterus, the alveoli in the lung are filled with fluid. When the baby is born, the sudden change in environment and drop in temperature make the baby to take a deep breath. The fluid in the lung is reabsorbed and replaced with air.
During expiration, the alveoli is prevented from collapsing by the surfactants.. If surfactant is deficient, the alveoli collapse which in turn produces hypoxemia, CO2 retention, etc.
When the alveoli collapse the damaged cells (alveolar cells, red blood cells, white blood cells and macrophages) collect and form a membrane like structure called Hyaline membrane which prevents gas exchange.
How RDS is diagnosed?
Diagnosis can be done either prenatally (before birth) or postnatally (after birth)
Prenatal (before birth): amniotic fluid index like Surfactant / albumin ratio, Lecithin / sphingomyelin ratio and presence of phosphatidyl glycerol (PG).in amniotic fluid.
Postnatal (after birth): through clinical signs and diagnostic tests.
What are the clinical signs of Respiratory Distress Syndrome?
- Increased respiratory rate
- Expiratory grunting (sounds like baby crying)
- Retraction (pulling inward of respiratory muscles) substernal, suprasternal and xiphoid
- Nasal flaring (widening of nostrils)
- Bluish discoloration (cyanosis)
What investigations (diagnostic tests) are done to diagnose RDS?
Oxygen saturation, Arterial blood gas analysis (ABG), routine blood investigations and blood sugar were done. X ray chest, echocardiogram and MRI chest can be done.
X ray findings in Respiratory Distress syndrome
X ray chest shows bell shaped chest, reduced lung volume and air bronchogram Staging
- Stage 1- infiltrates
- Stage2 – infiltrates with reticulogranular pattern
- Stage3- reticulogranular pattern extended and blurring the cardiac shadow
- Stage4- ground-glass opacity
What is the treatment (management) for Respiratory Distress Syndrome?
Start oxygen therapy and if necessary, support respiration with noninvasive ventilation like CPAP or intubate the baby and start mechanical ventilation.
Surfactant replacement therapy: Animal derived (bovine) or synthetic surfactant can be administered through endotracheal tube. Early CPAP and surfactant administration may reduce death rate (mortality), air leak and other complications. This can be continued till the baby produces enough surfactant.
Plan of care
Supportive management includes maintaining normal body temperature, adequate fluid, acid-base balance, and proper nutrition
Prevent infections by proper vaccinations.
What are the complications of RDS?
- Pneumothorax
- Broncho Pulmonary Dysphagia
- Pulmonary hemorrhage
- Intra Ventricular Hemorrhage
Respiratory Distress Syndrome (RDS) in Neonates Read More »
Arterial Blood Gases (Arterial Blood Gas Analysis)

What is meant by Arterial Blood Gas analysis?
An arterial blood gas analysis is a procedure (test) that is performed to measure oxygen, carbon dioxide and acid/base status (pH) in arterial blood.
What are the terms used in Arterial blood Gas analysis?
- PaCO2: ( ventilation ) partial pressure of carbon dioxide
- PaO2:(oxygenation) partial pressure of oxygen
- HCO3: ( metabolism ) bicarbonate
- SaO2 : Oxygen saturation
- pH : ACID/BASE balance
Why Arterial Blood Gas test is done?
Arterial Blood Gas analysis is done in critically ill patients to assess the need for mechanical ventilation.
- Arterial Blood gas analysis is done for the patients under mechanical ventilation in order to check and review the oxygenation status of the patient and provide further treatment according to the defects.
- To give anesthetic fitness in patients who cannot perform spirometry or PEFR.
- In the case of thoracic trauma or any other open heart surgeries to find out whether ventilator is required or not.
- Sudden difficulty in breathing (dyspnoea)
- Cyanosis (bluish discoloration of finger tips, lips &tongue)
- Sudden tachypnea (increase in respiratory rate)
- Shock and sepsis
- In patient with respiratory disease, ABG analysis provides information about lung ventilation.
- In patient with metabolic disease and selected drug overdose are at risk for acid base abnormalities, diagnosed through pH, PCO2 and HCO3 levels.
What are the contraindications for ABG Testing?
- If the patient has inadequate collateral circulation at puncture site
- Infection or any other lesions at the site of puncture
- Burns over the site
- Coagulopathy (problem in blood clotting)
- Arteriovenous fistula (abnormal connection between artery and vein)
- Peripheral vascular disease at the artery site.
- Patients taking anti coagulants.
What are the complication of ABG analysis?
- Hematoma
- Hemorrhage
- Numbness of hand
- Infection
- Air embolism
- Thrombus embolism
HOW TO PERFORM ABG TEST?
- FIRST STEP: Prepare the equipments that are required for the procedure.
- SECOND STEP: Make the patient comfortable and explain the procedure
- THIRD STEP: Perform Allen’s test, before starting the procedure.
What are the Equipments required?
- Syringes
- 22 -23 gauge needle
- Alcohol swab
- Heparin
- Cotton
- Gloves
- Gauze pad
Which is the common site from where blood is collected?
- Radial artery: It is the most common site because of the presence of collateral circulation and easy to access. The complications like bleeding and hematoma formation can easily noted.
- Brachial artery
- Femoral artery
- Dorsalis pedis artery
- Posterior tibial artery
What is Allen’s test?
Allen’s test is done to ensure that there is good collateral circulation available from ulnar artery, if radial artery is damaged during the procedure.
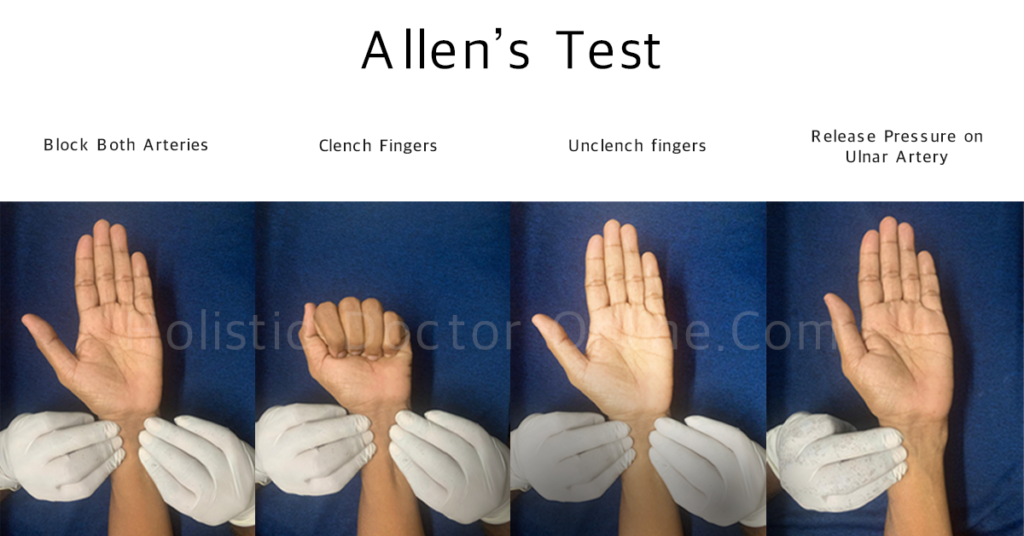
How to perform Allen’ s test?
- Make sure that you wash your hand and wear gloves before doing the procedure.
- Introduce yourself and explain the procedure that is going to be done for the patient and make them comfortable.
- Make sure that you obtain the consent from the patient.
- To perform Allen’s test, first instruct the patient to close their hand tightly and the therapist should compress both the radial and ulnar artery.
- Later the patient is instructed to open his /her hand as the therapist releases the pressure on the ulnar artery.
- The hand should turn to pinkish color within 10 to 15 seconds, if it is so then there is good collateral circulation and you can perform the test
- If the color is not restored within 10 to 15 seconds then that means there is no collateral circulation and should avoid the test in that hand and start performing the test on the opposite hand.
Procedure
- After performing the Allen’s test
- Place a folded towel or a bottle under the patients wrist, so that it keeps the wrist hyper extended
- Clean the site using an alcohol swab
- Attach the needle to the heparinised syringe
- Feel the pulse of the radial artery with your index and the middle finger.
- Once you start feeling the pulse, fix the artery and Insert the needle at 45 degree angle to the skin, advance the needle in to the artery until the blood flushes into the syringe.
- The arterial pressure will cause the blood to fill the syringe.
- Remove the needle slowly; a gauze pad or cotton should be applied with pressure over the puncture site for at least 5 minutes.
- Cap the syringe safely and make sure to push the air out.
- And send the sample immediately for analysis
- Remove the gloves and dispose it and thank the patient.
How the ABG results are interpreted?
Normal Values:
pH: 7.35 to 7.45 and absolute normal pH is 7.4.
PaCO2: 35 to 45 mmHg.
HCO3: 22 to 28 m mol/L.
PaO2 : 80 to 100 mm Hg.
SaO2 : 95 to 100%
How to determine whether it is acidosis or alkalosis?
Acidosis:
When pH is decreased, (less than 7.35)
When PaCO2 is increased (more than 45 mm Hg),
When HCO3 is decreased (less than 22 m mol/L)
Alkalosis:
When pH is increased (greater than 7.45)
When PaCO2 is decreased (less than 35 mm Hg)
When HCO3 is increased (more than28 m mol/L)
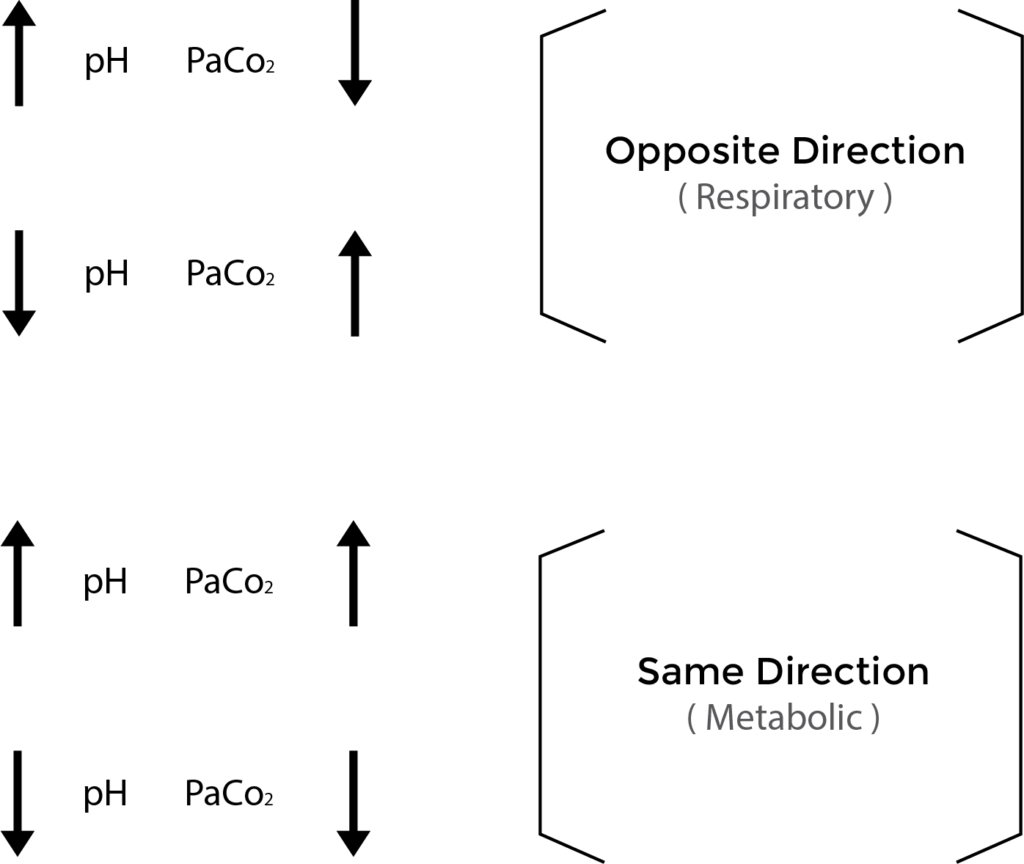
How to determine whether the acidosis/ alkalosis is due to respiratory or metabolic cause?
Think of ROME to know whether the cause is respiratory or metabolic.
RO: Respiratory opposite- in respiratory acidosis or alkalosis, the pH and PaCO2 values move in the opposite direction.
ME: Metabolic Equal – in metabolic acidosis or alkalosis, the pH and PaCO2 values move in the same direction.
What is meant by compensation?
When the chemo receptors in our body senses the change in pH, our body tries to compensate (correct and balance) it by adjusting the rate and depth of respiration or by making the kidney to adjust H+ secretion and re absorption of bicarbonate.
Example: When respiratory acidosis (low pH with high PaCO2) develops the kidneys try to compensate it by increasing bicarbonate re absorption and increase carbonic acid excretion.
Arterial Blood Gases (Arterial Blood Gas Analysis) Read More »
Pulmonary Interstitium and Interstitial lung disease
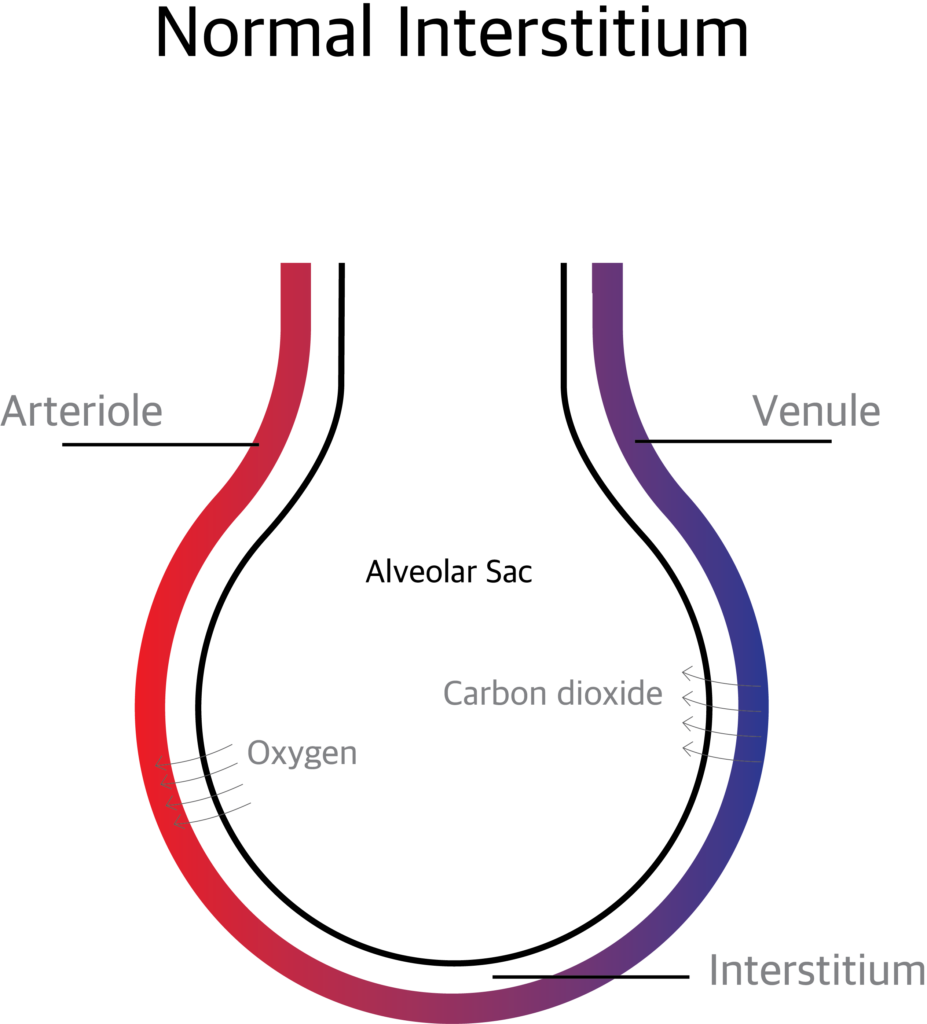
What is pulmonary Interstitium?
The Pulmonary Interstitium is the anatomical space between the alveolar epithelial cells and the endothelium of the pulmonary capillaries. It continues as the space surrounding the bronchi and blood vessels. The interstitium contains perivascular and peri lymphatic tissue.
What are the sub divisions of Pulmonary Interstitium?
The pulmonary interstitium is divided in to 3 components.
The Axial (peri bronchovascular) Interstitium: The space around the airways and the pulmonary artery.
The Parenchymal or Alveolar Interstitium: The interstitium supporting the gas exchanging part of the alveoli.
The Pheripheral or Sub pleural Interstitium: The space between the parenchyma of lung and the visceral pleura.
What are the functions of pulmonary Interstitium?
The pulmonary Interstitium supports the alveolar sacs and transport nutrients. The exchange of oxygen and carbon dioxide takes place through the pulmonary interstitium.
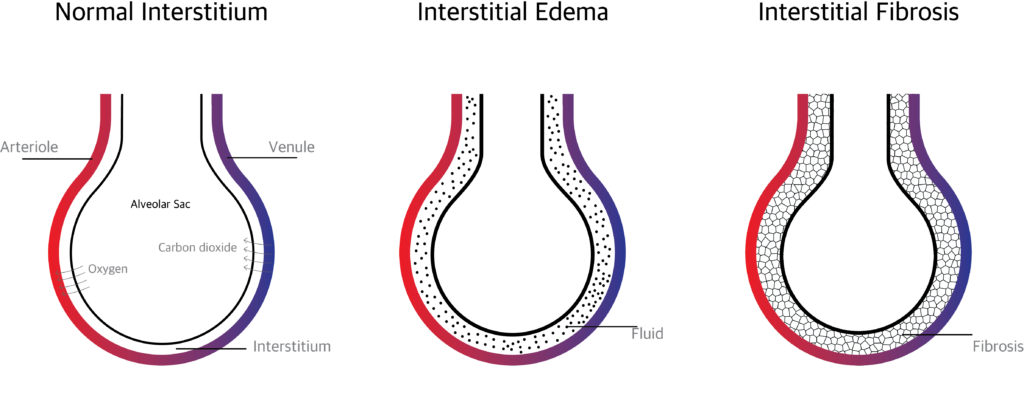
The gas exchange is affected when excess extra vascular fluid accumulates in the interstitium or when the interstitium is affected by inflammation and scaring.
Disorders of pulmonary Interstitium ( Interstitial lung disease)
What is Interstitial Lung Disease (ILD)?
Interstitial lung disease is a collection of more than hundred disorders affecting the pulmonary Interstitium.
What is the pathophysiology of Interstitial Lung Disease?
Normally when there is an infection and inflammation, the interstitium will heal shortly with minimal or no scaring. Repeated insult and infection over times makes the interstitium thick and hard. This hardened interstitium becomes a barrier between the alveolar membrane and blood vessels thereby preventing gas exchange.
What are the causes of Interstitial Lung Disease?
There are more than hundred causes. The causes may be known, unknown or hereditary.
Known Causes:
- Granulomatous infections (like tuberculosis, mycoplasma), viral and fungal infections can cause interstitial lung diseases.
- Hypersensitivity pneumonitis:- Dust, molds, animal or birds proteins (Feathers or droppings) can irritate and produce scarring of the interstitium.
- Pneumoconiosis:- occupational hazards like breathing asbestos fibers (Asbestosis) or Silica dust (silicosis), cotton fibers (byssinosis) Sugarcane fibers and mold (bagassosis) etc can cause ILD.
- Toxic pneumonitis:- Inhaling chemicals, fumes or drugs can develop ILD. Exposure to radiation can also produce ILD.
- Drug induced:- Ingesting drugs like Nitrofurantoin, bleomycin, propranolol, amiodarone and rituximab can cause ILD.
- Malignancy:- Neoplasms like bronchoalveolar cell carcinoma and lymphangitic carcinomatosis can produce ILD.
- Respiratory bronchiolitis:- caused by chronic smoking can also produce ILD.
Unknown causes:
- Crptogenic Organizing pneumonia:- otherwise called as bronchiolitis obliterans organizing pneumonia (BOOP)
- Idiopathic pulmonary fibrosis
- Sarcoidosis:- involves lymph glands, other organs like skin heart etc, and interstitium.
- Langerhans cell histocytosis
- Eosinophilic pneumonia
- Pulmonary alveolar proteinosis
- Pulmonary vasculitis;- Eg: wegener’s granulomatosis.
- Lymphangioleiomyomatosis
- Connective tissue diseases like Rheumatoid Arthritis, Progressive systemic Selerosis etc…
Inherited (hereditary) causes:
- Neurofibromatosis
- Tuberous sclerosis
- Metabolic storage disorder
- Hypocalciuric hypercalcemia
- Hermanszky-pudlak syndrome
What are the signs and symptoms of Interstitial Lung Disease?
Symptoms:
The main symptom is gradually increasing breathlessness on exertion and finally breathlessness even at rest.
Cough usually dry, weight loss, general weakness and fever when there is super added infection.
Signs:
Digital clubbing,
Velcro crackles on auscultation.
How to diagnose ILD?
Detailed history regarding occupation, exposure to dust, chemicals, drugs, family history, and personal history (smoking, drugs etc) has to be taken. In ILD is suspected the following investigations have to be done.
What are the tests (investigations) done in interstitial lung disease?
- Routine investigations like complete blood count, ESR, Blood sugar etc were done.
- Serological tests like Antinuclear Antibody Test, Creatine Kinase, Rheumatoid Factor etc… are done to rule out connective tissue diseases.
- X- Ray chest
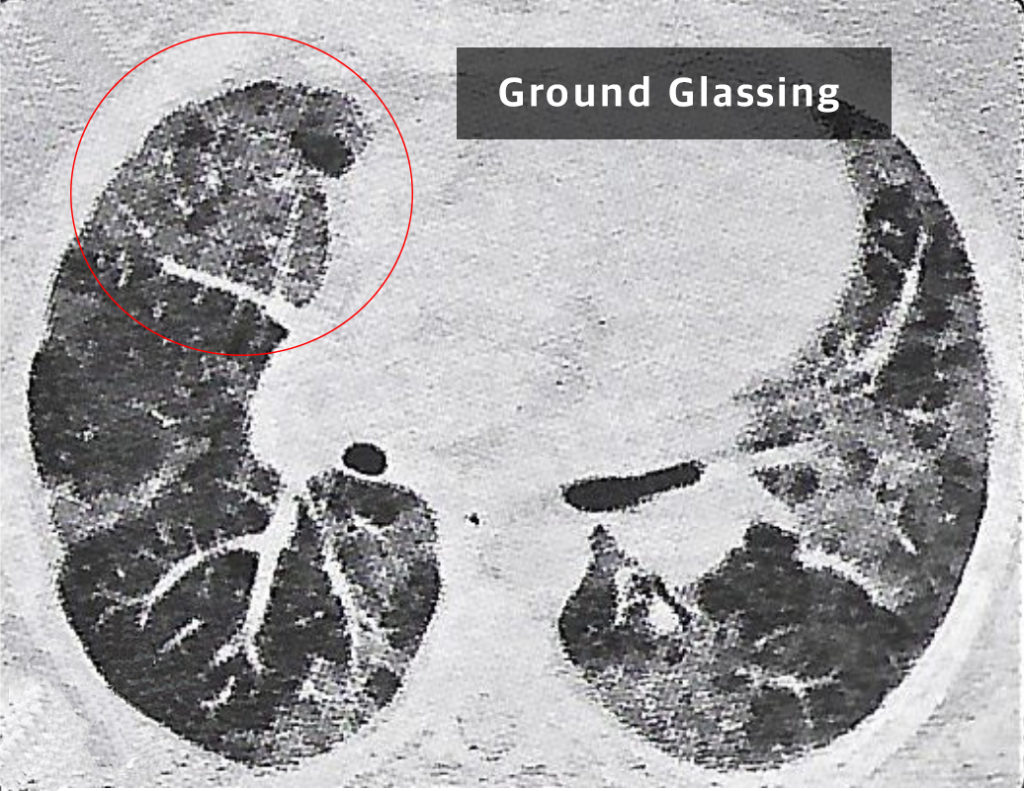
- HTCT thorax: Patchy peripheral opacities are seen. Bronchiectatic changes and sub plural reticular opacities seen. Limited ground glass opacities are seen.
- Sputum examination, culture and sensitivity testing
- Spirometry: Restrictive pattern
- Six minutes walk test bronchoscopy and broncho alveolar lavage: specimen sent for cell count, cytology, culture etc.
- Lung Biopsy: Trans bronchial biopsy (TBLB) or Video assisted thoracoscopic biopsy (VATS)
What is the treatment for interstitial lung disease?
Treatment is based on the diagnosis. If due to known cause treat the cause.
If the cause is not known, the goal of the treatment should be to reduce symptoms, to improve the quality of life and to reduce complications.
Response of treatment varies. Some may recover well and some may not.
The treatment options are:
- Corticosteroids: Corticosteroids like prednisone reduce inflammation. Oral Steroids are initially used to reduce inflammation but in later stages steroids may not be effective.
- Immunosuppressive drugs: Azathioprim or Cyclophosphamide or Mycophenolate can be given when steroids are not effective.
- Antifibrotic agents: Pirfenidone, Colchicine, D-pencillamine, Interferon Y or B, Suramin, Nintedanib etc can be given to reduce scarring.
- Antioxidants: N-acetyl cystein, Niacin, Glutathione, etc can slow down the progress of the disease.
- Long term oxygen therapy: Some people may need long term oxygen therapy. Oxygen concentrator can be advised.
- Pulmonary Rehabilitation: Pulmonary rehabilitation given to the patient to make him live independently in the society. Pulmonary rehabilitation includes health education, exercises, breathing techniques, occupational therapy, counselling and psychosocial support.
- Lung Transplant: In end stage ILD, when other treatment options are not effective lung transplant can be tried.
Pulmonary Interstitium and Interstitial lung disease Read More »
Tracheal Extubation
What is Tracheal Extubation?
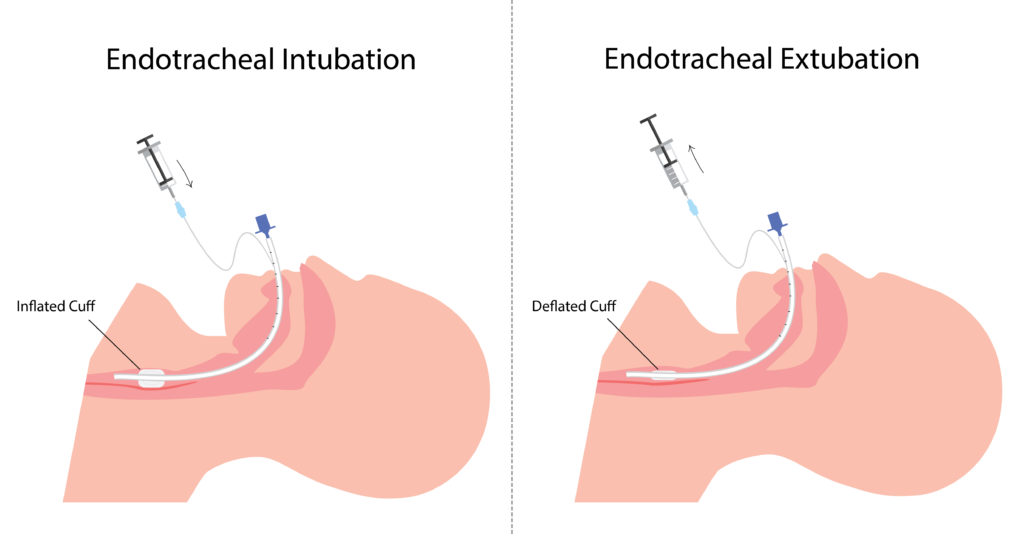
Endotracheal tube is a flexible polyvinyl chloride tube which helps to assist breathing. The process of placing endotracheal tube in the airway is called Intubation. Intubation is done to provide artificial breathing. Tracheal extubation is the process of removing the endotracheal tube from the airway.Extubation is done, once the patient is weaned (gradual withdrawal) from the ventilator.
What are the indications for Tracheal Extubation?
When the patient has improved and no longer need artificial airway to breathe. If the patient is maintaining adequate gas exchange, perfusion and have improved breathing pattern and cardiovascular status.
If the patient is having improved airway protective mechanism such as cough to clear the secretions. The need for exchange of ET tube due to mucus and other secretion obstruction.
What are the contraindications for Tracheal Extubation?
In patients who cannot maintain clear airway.
In patients who have weak respiratory muscles, inadequateventilation and perfusion.
In patients who have persistent hypoxia and hypercarbia.
In patients who have severe cardiac instability, hypothermia andmetabolic imbalance.
What are the criteria for Tracheal extubation?
Before Extubation, Spontaneous Breathing Trial (SBT) is done to assess the capability of the patient to breathe in a minimum ventilatory support and oxygen support. In SBT, patient should complete 30 to 120 minutes with low level of Continuous positive airway pressure (CPAP) pressure support, showing normal breathing pattern, cardiovascular status and gas exchange.
Subjective assessment for Extubation
Adequate cough.
No neuromuscular blockers and sedatives.
Absence of excessive and thick secretions.
Improvement in disease condition.
Objective measurement for Extubation
Stable cardiovascular status.
Heart rate≤ 140 b/min.
No active myocardial ischemia.
Adequate hemoglobin levels ( ≥ 8g /dl).
Systolic blood pressure 90-160 mmhg.
Afebrile.
No or minimal vasopressor or inotrope.
Oxygenation assessment for Extubation
Tidal volume > 5ml / kg.
Vital capacity 10ml / kg.
Proper inspiratory effort.
Respiratory rate≤35minutes.
Rapid shallow breathing index<105.
PaO 2 ≥60 and PaCO 2 ≤60 mmhg.
PEEP ≤ 8cm h2O.
No significant respiratory acidosis ( PH ≤ 7.30).
Maximal inspiratory pressure (MIP) ≤‐20 – – 25 cmh2O.
O 2 saturation > 90% on FiO 2 ≤ 0.4.
What is Cuff Leak Test?
Cuff leak test is done before Extubation to check the presence of laryngeal edema which is one of the major causes of respiratory failure which leads to reintubation.
Test procedure for cuff leak test
The cuff is completely deflated with a 10ml syringe and tidal volume is measured.
Cuff leak calculation ;
Tidal volume before deflation- Tidal volume after deflation= cuff leak
The percentage of cuff leak should be 15%
It low cuff leak is detected the patient has edema.
Intravenous or nebulized corticosteroids and epinephrine are administered to treat the above conditions.
What are the equipments needed for Tracheal extubation?
All the equipments needed for the intubation must be checked and arranged, because in some cases reintubation may be required or respiratory failure may occur.
Important equipments for Extubation
Suctioning equipment
Scissors
10ml syringe
Bag valve mask resuscitator
Supplemental O 2
O 2 mask or NIV according to patients need
Crash cart
What is the procedure for Tracheal Extubation?
- Complete suctioning of upper airway and ET tube to prevent the entry of secretions in to the lower airway.
- The patient should be bagged with 100 % oxygen.
- The cuff is completely deflated using a syringe
- Remove the ET tube holder or tapes.
- Remove the ET tube;
A large breathe was given through the bag valve mask resuscitator, the tube is removed during maximal inspiration where the vocal cords are in open position.
The patient is encouraged to cough; the tube is removed at the expulsive expiratory phase where the vocal cords are in maximal open stage. - Oxygen therapy or NIV is provided according to the patient’s need.
- Auscultation is done to assess the presence of stridor or decreased air entry.
- The patient’s ABG values are checked. Heart rate, blood pressure, saturation should be continuously monitored.
What are the complications of Tracheal Extubation?
Common complications:
Hoarseness of voice
Sore throat
Cough
Other complications are,
Hypoventilation
Increased work of breathing
Respiratory muscle weakness
Aspiration due to improper suctioning
Pulmonary edema
Bronchospasm
Atelectasis
Laryngospasm
These complications of Extubation may lead to extubation failure.
What is Extubation failure?
When re-intubation is necessary within 24-48 hours of planned Extubation then it is called Extubation failure.
Non invasive ventilation (NIV) helps to reduce the chances of Extubation failure.
Tracheal Extubation Read More »
Lung Expansion Therapy
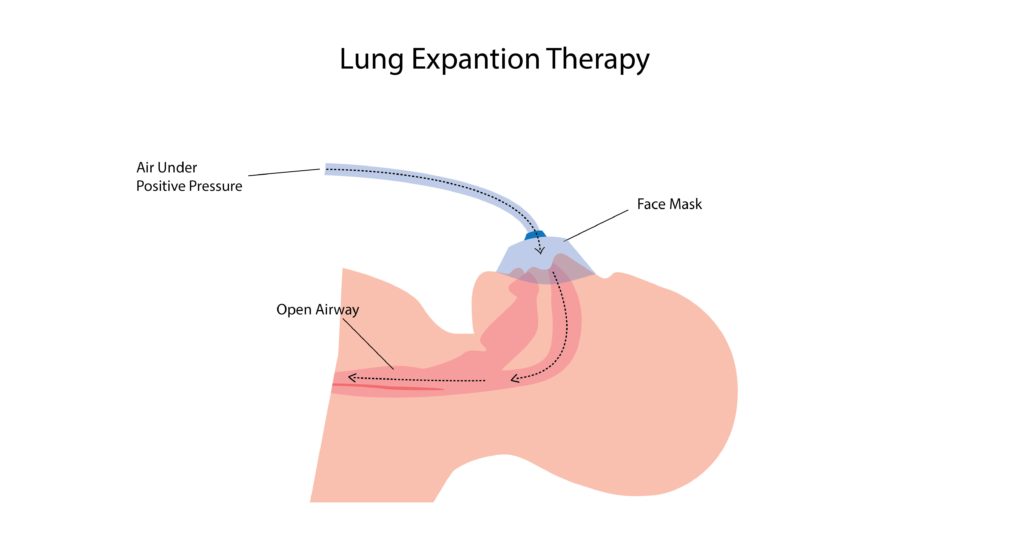
What is lung expansion therapy?
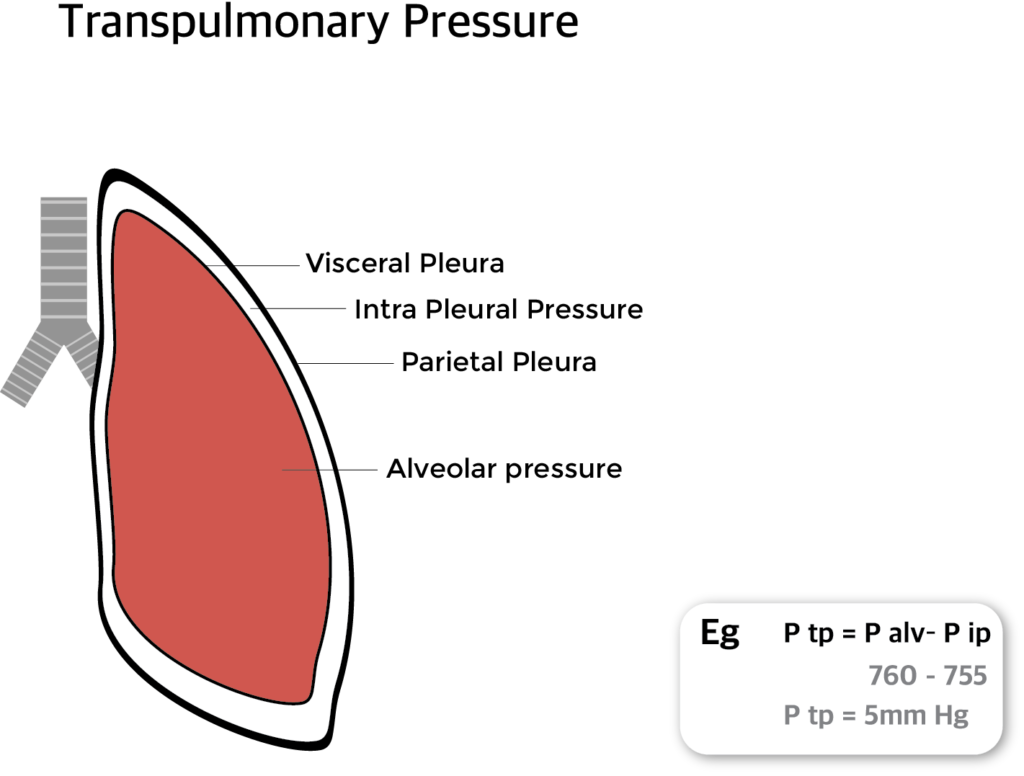
Lung expansion therapy includes many techniques to improve pulmonary function by increasing alveolar recruitment (open collapsed alveoli) and airway clearance. It increases lung volume by increasing the pressure difference between the alveolar space and pleural space (transpulmonary pressure).
Expansion of the collapsed lung can be obtained by deep breathing exercises or by applying positive pressure using devices like Incentive spirometer, CPAP, PEEP, Bi PAP, IPPB etc.
What is transpulmonary pressure?
Tran pulmonary pressure (P tp) is the difference between the alveolar pressure (P alv) and intra pleural pressure (P ip).
P tp = P alv– P ip
Transpulmonary pressure can be increased by
- Decreasing the surrounding pleural pressure
- Increasing the alveolar pressure
What are the indications for lung expansion therapy?
- Presence of alveolar collapse ( atelectasis)
- Conditions predisposing to atelectasis ( chronic bedridden patients)
- Upper abdominal or thoracic surgery
- Patients with neuromuscular disorders
- Sleep apnoea
- Surgery in patients with COPD
- Presence of restrictive lung disease.
What are the Contraindications for lung expansion therapy?
- Unconscious patients and un cooperate patients
- Patients who cannot understand and follow the instruction
- Patients unable to take deep inspiration, eg: Vital capacity <10 mL/kg or IC <1/3 predicted normal
What are the Complications Of lung expansion therapy?
- Hyperventilation and respiratory alkalosis
- Discomfort due to inadequate pain control
- Barotraumas
- Hypoxemia (with interruption of therapy)
- Exacerbation of bronchospasm
- Fatigue
What are the techniques of lung expansion therapy?
Lung expansion therapy consists of a variety of respiratory care techniques designed to prevent or correct Collapse of lung (atelectasis).
The most common techniques include
- IIncentive spirometry (IS),
- continuous positive airway pressure (CPAP)
- positive expiratory pressure (PEP)
- Intermittent positive airway pressure breathing (IPPB)
These techniques help the patient to improve pulmonary function by increasing alveolar recruitment and airway clearance.
What is Incentive spirometer?
Incentive spirometer is a device which helps the patients to improve their lung function. The patient has to take a slow and deep breath, hold the breath for 5 to 6 seconds (sustained maximal inspiration) and then breathe out. This pressure helps to open the collapsed alveoli and airway.
What is IPPB?
IPPB (Intermittent positive pressure breathing) therapy is a technique used to expand the collapsed lung. Here inspiratory positive pressure is delivered in to the airway of a spontaneously breathing patient on an intermittent (short-term) basis by a trained respiratory therapist (RT). In IPPB a preset positive pressure is delivered only during the inspiratory phase of respiration.
This pressure helps the patient to take deep breath which in turn opens the collapsed lung and airway. IPPB is also used to improve cough mechanism, dislodge secretions and enhance delivery of inhaled medications.
Positive Airway Pressure Therapy
In positive airway pressure therapy compressed air in a preset pressure is delivered in to the airway which keeps the lung and airways open.
What are the types of Positive Airway pressure therapy?
- Positive expiratory pressure (PEP)
- Expiratory positive airway pressure (EPAP)
- Continuous positive airway pressure (CPAP)
- Bi level positive airway pressure (Bi PAP)
CPAP (Continuous Positive Airway Pressure) Therapy
It is a positive airway pressure therapy where a preset continuous pressure is maintained in the airway throughout inhalation and exhalation thereby preventing collapse of alveoli and airways.
CPAP is mainly used in obstructive sleep apnoea.
Bi PAP (Bi level positive airway pressure) therapy
In Bi PAP therapy different level s of pressure are maintained during inspiration and expiration. Usually a pressure around 8 to 12 cm of water (H2O) is maintained during inspiration and pressure around 2 to 4 cm of H2O is maintained during expiration.
Bi PAP is a type of non invasive type of mechanical ventilator. It is usually used in patients with COPD and patients with respiratory distress and in Obstructive Sleep Apnoea patients where CPAP is not effective.
PEP therapy
In PEP (Positive Expiratory Pressure) Therapy the patient is made to breath out (Exhale) against resistance through a PEP device. The pressure created is transmitted to airways, creating a back pressure which prevents collapse and keep the airways open during exhalation.
PEP therapy prevents collapse of lung and airways, prolong expiratory flow and promote airway clearance.
Patient has to inhale, hold the breath and exhale through the PEP apparatus. A pressure around 10cm of water is maintained at mid expiration.
EPAP therapy
EPAP (Expiratory Positive Airway Pressure) therapy works by creating pressure during expiration and keeping the airway open until n inspiration. It is a simple, non invasive and effective treatment for obstructive sleep apnoea.
EPAP device consists of 2 two way valves one for each nostril. On inhalation the valves open and allow air to enter freely and on exhalation the valves restricts air flow. This restriction increases pressure inside the airway and prevents collapse of airway.
The EPAP device is small, portable, not attached to any machine and no need for power supply. Airway Pressure (EPAP) which is maintained until the start of the next inspiration.
Lung Expansion Therapy Read More »
Causes, Symptoms, Diagnosis and treatment of bronchiectasis
What is bronchiectasis?
Bronchiectasis is an abnormal irreversible (permanent) dilatation of some bronchi or bronchioles (enlargement of parts of airway).
What are the causes of bronchiectasis?
The main cause of bronchiectasis is frequent, chronic lower respiratory tract infections like tuberculosis, haemophilus influenza, streptococcus, klebsiella etc. Bronchiectasis can occur as a complication of Cystic Fibrosis. A congenital (hereditary) condition called Kartageners syndrome where there is defect in ciliary function can also produce bronchiectasis.
What is the pathogenesis of bronchiectasis?
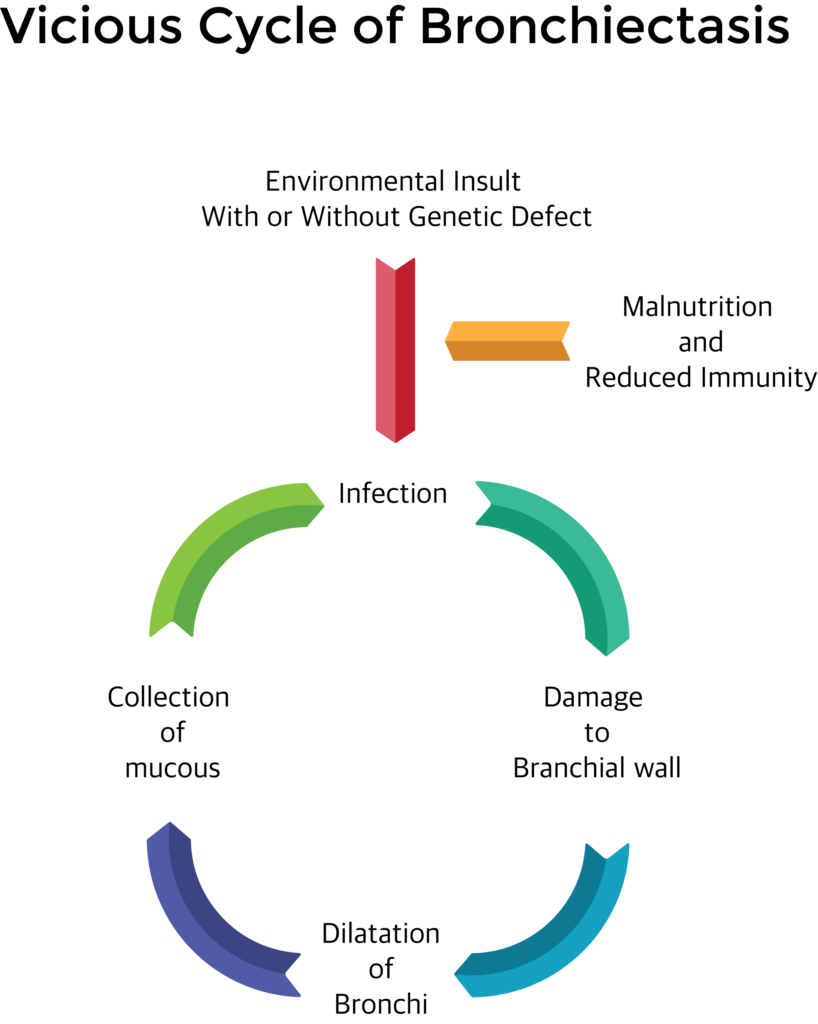
Chronic infections may damage the mucosal layer and mucociliary clearance. Inflammatory cells infiltrate leading to sloughing and ulceration in the wall of the bronchi. This may lead to patchy scarring and dilation of the area of bronchi. In the dilated area mucous gets collected which in turn gets infected and produce further damage.
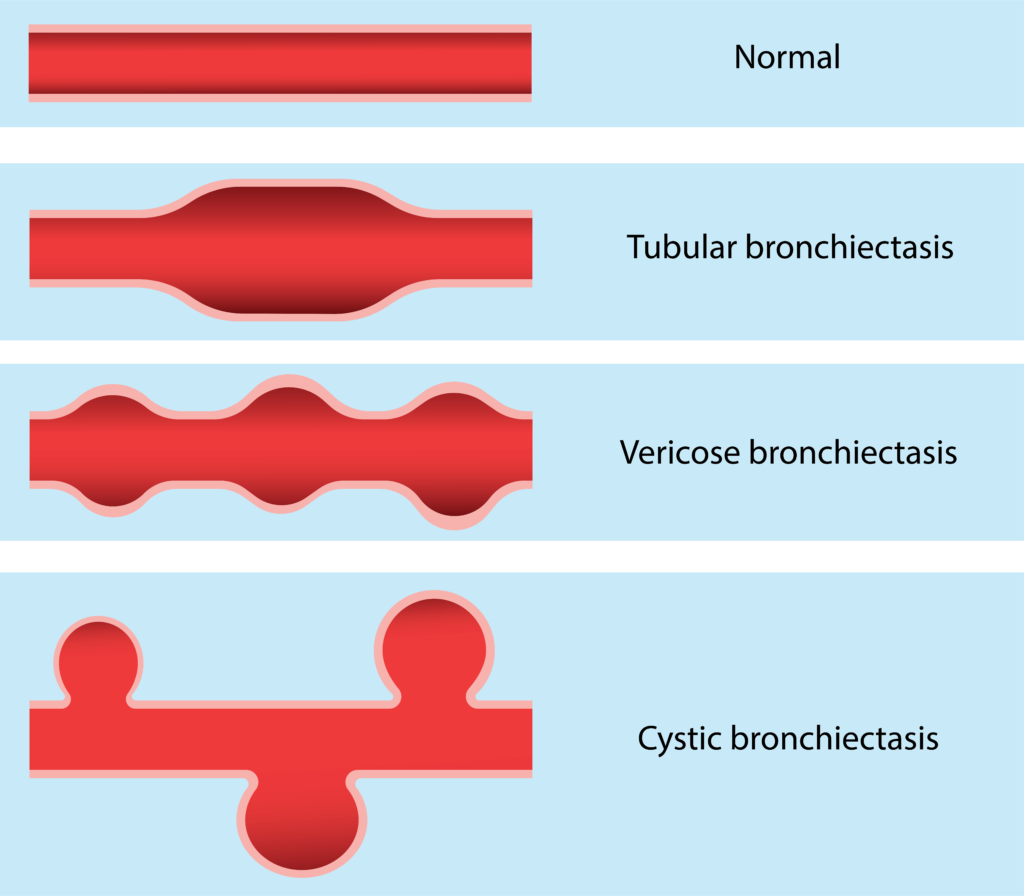
What are the types of bronchiectasis?
According to the shape of dilatation, there are three types of bronchiectasis. They are cylindrical, tubular and varicose.
What are the symptoms and signs of Bronchiectasis?
Symptoms
- Cough with copious (lots of), thick, foul smelling sputum.
- Haemoptysis (Blood in sputum)
- Shortness of breath, chest pain
- Fever with or without chills
Signs
- Halitosis (foul smelling breath)
- Labored breathing: patient using accessory muscles for breathing.
- Clubbing of fingers
- Coarse crackles (Crepitations) on auscultation.

How to diagnose Bronchiectasis? (investigations)
X ray chest: increased bronchovascular markings, multiple cysts containing fluid levels.
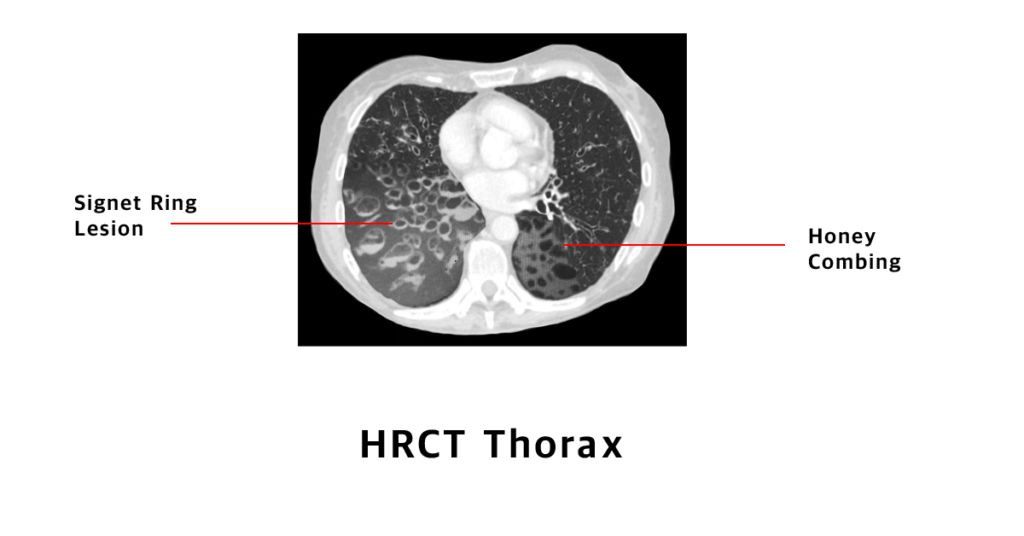
HRCT scan chest: Signet ring lesions, honey combing with fluid levels.
Sputum test for gram stain and acid fast stain.
Sputum for culture and drug sensitivity testing,
Routine blood tests like bloodcount, ESR, Bloodsugar,
Bronchography or bronchoscopy.
What is the treatment for bronchiectasis?
Postural drainage and chest physiotherapy.
Antibiotics: Start with broad spectrum antibiotics and can be changed according to the drug sensitivity.
Bronchodilators and expectorants,
Airway clearance devices,
Reassurance and health education.
Surgical excision: Very rarely done when bronchiectasis is localized and with severe haemoptysis.
How to prevent Bronchiectasis?
Diagnose and treat respiratory tract infections early.
Vaccinations schedule to be followed in children and adults can take pneumococcal vaccine like PISV 23 or PCV 13.
Prevent malnutrition by taking well balanced high protein diet.
Causes, Symptoms, Diagnosis and treatment of bronchiectasis Read More »
Respiratory therapist
Who are called respiratory therapist?
Respiratory therapist also called as respiratory care practitioners are paramedical professionals who basically deals with the problems related to lungs and airways of an individual from their first breath till the very last breath i.e., all age group of patients who has a simple cough or someone who require I.C.U care. The Respiratory Therapist can help them as an individual or as a part of multidisciplinary team to improve the health related quality of the patient.
Where can respiratory therapist work inside a hospital?
Respiratory Therapist can work in coordinate with physicians in order to formulate individual care for patients depending upon their respective disease condition i.e., in co-ordination with Pulmonologist, Pediatricians, Anesthetist, Critical Care Medicine, Emergency Medicine, or even in pre and post operative care as a backup for Surgeons to restore ventilation. In a hospital, they can work in outpatient department, inpatient department, critical care unit, pulmonary rehabilitation centre and pre or post operative care unit.
What is the role of respiratory therapist ?
The vital role of Respiratory Therapist is to assess, aid in diagnose or treat and care for patients with cardiopulmonary disorders. They play a vital role as a member in Code blue team (Cardio Pulmonary Resuscitation) to restore ventilation to the lungs, which includes a vast category of patients from newborns to elderly.
Under Pulmonology / Critical Care Medicine or Emergency Medicine
Respiratory therapist takes a brief history of patients, perform some physical examination and also help in diagnosis of the patient’s disease with the help of certain equipments.
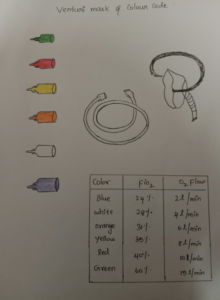
- Respiratory Therapist may use oxygen alone or in combination with other gases and chose appropriate device for their delivery depending upon the patients need.
- Provide aerosol medication with medical devices such as nebulizers for patient with breathing difficulty depending on patient need and understanding in coordination with the physician
- For patients who are unable to clear their secretion or who cannot cough well, the respiratory therapist will provide Chest Physiotherapy which has various methods.
- Diagnostic tools such as Spirometry are used to measure the lung capacity. So that treatment plan can be made accordingly.
- Ventilator management: Disease like pneumonia may require extra concentration of oxygen with or without pressure to improve breathing. Respiratory Therapist aids the patient by providing them the right amount of oxygen with the appropriate device.
- Pressured oxygen can be delivered to the lung with a help of endotracheal tube which directly enters the lung via windpipe/ trachea and is connected to a pressured oxygen delivery device called ventilator. This can be also given through simple face mask which is called non invasive ventilator. Alteration are made with the help of blood analysis which will be done every now and then by Rt’s also with regular check on patient condition and their equipment used in accordance with physicians order.
- They also help victim in special scenarios like heart attack, choking, drowning or shock. In home care setting, Respiratory therapists teach patients and their family members to use their respiratory care equipments in the correct way. In addition, they also have scheduled visits to check the patient in home to modify the plan in accordance with their status of disease.
- Respiratory Therapists have expanded their area of work by involving them self in multidisciplinary team and work with physicians in case management, pulmonary rehabilitation, and counseling for smoking cessation, Disease prevention and also trained in Polysomongraphy (diagnostic tool for sleep diseases).
- In newborn care, the respiratory therapists has to aid in flushing out the fluid from the lungs either by stimulation or with the use of artificial ventilation devices which results in lung function of newborns.
How long will they work and how much is their salary?
Respiratory Therapist generally work around 35-40 hours a week. Depending upon their work place this time may vary. Average salary ranges around Rs 18,000- 25,000/ month depending field of interest and work area.
Conclusion
Most of the Respiratory therapists must complete a 2-4 year program of study and can register in IARC (Indian Association of Respiratory Care). In short Respiratory Therapists provide both temporary relief and permanent solution to patients suffering from disorders related to lung and airways of all age group. The goal of the respiratory therapist is to help the patient to breathe with comfort.
Respiratory therapist Read More »
Cystic Fibrosis Causes, Signs, Symptoms and Treatment.
What is Cystic Fibrosis?
Cystic Fibrosis is a hereditary disease caused by gene mutation (alteration in gene sequence and structure). The mutation occurs in the gene for the CFTR protein (cystic fibrosis Trans membrane Conductance Regulator) on chromosome 7.
The main feature of Cystic Fibrosis is an abnormal high level of sodium and chloride in secretions of exocrine glands.
Cystic Fibrosis is seen in new born babies and seen in 1 in 2000 live births.
What are the organs affected by cystic fibrosis?
Cystic fibrosis mostly affects the lungs. It can also affect secretory organs like sweat glands, digestive system, pancreas and liver.
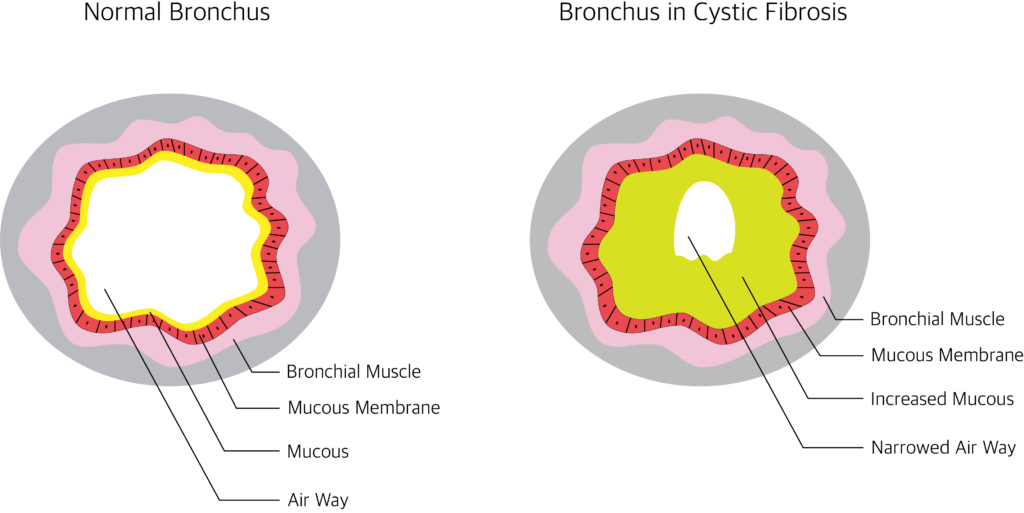
How Cystic fibrosis affects the lungs?
Because of the abnormal composition of sodium and chloride the mucus becomes thick and sticky. This impairs the mucociliary clearance. This leads to chronic infections and further leads to bronchiectasis, emphysema etc.
What are the signs and symptoms of Cystic Fibrosis?
Symptoms
Respiratory system
- Cough with sputum
- Wheeze
- Repeated lung infections
- Exercise intolerance
- Recurrent sinusitis
- Nasal polyps
Other organs
- Fatty liver or cirrhosis
- Diabetes
- Gall stones
- Intestinal obstruction
- Intussusception
- Infertility
Signs
In neonates: Meconium ileus, failure to thrive, rectal prolapse and distended abdomen.
In adults:
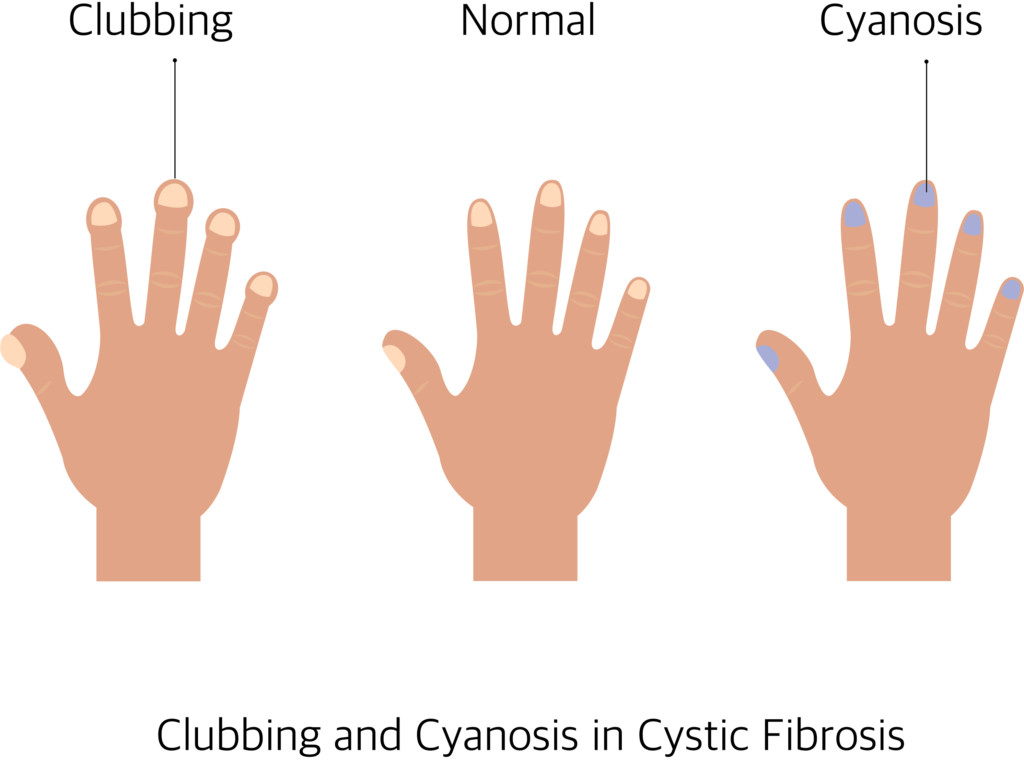
Clubbing: Tips of toes and fingers are enlarged.
Cyanosis: Bluish discoloration of nail, lips and tongue.
Bilateral coarse crackles heard over lung field.
How to diagnose cystic fibrosis?
- Sweat sodium and chloride test: It measures the salt in your sweat. The mean concentration of sodium and chloride in sweat is 20 to 35mmol/l. values above 70 mmol/l is suggestive of cystic fibrosis.
- Blood tests: Check the level of immune reactive trypsinogen (IRT) .The people with cystic fibrosis have higher level of immune reactive trypsinogen in their blood. Routine blood tests like blood sugar, liver function test, and kidney function tests are done.
- Sputum gram stain, culture and drug sensitivity testing.
- DNA test: To look for the mutations to CFTR Gene
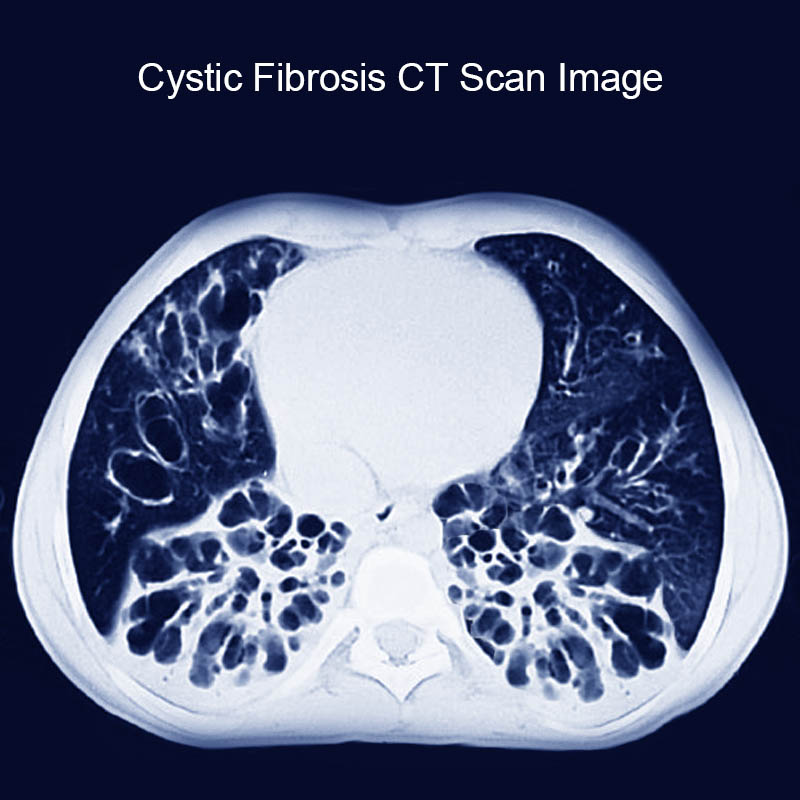
- Chest X ray and CT scan: Bronchiectasis or hyperinflation.
- Abdominal ultra sound scans to look for cirrhosis or fatty liver and chronic pancreatitis.
- Spirometry: Obstructive airway defect.
How to treat cystic Fibrosis?
Cystic Fibrosis cannot be cured completely. Treatment is aimed to reduce symptoms, slow down the progress of cystic fibrosis, prevent complications and to improve the quality of life.
Following treatments are given:
- Antibiotics
- Anti-inflammatory drugs (to prevent swelling)
- Bronchodilators
- Mucus thinner
- CFTR modulators
- Combination therapy
- Airway clearance techniques
- Oscillating devices
- PEP (positive expiratory pressure) treatment) using flutter or acapella PEP therapy.
- Pulmonary Rehabilitation, Nutrition.
What are the complications ?
- Bronchiectasis (damaged airway)
- Haemoptysis ( blood in sputum)
- Pneumothorax
- Respiratory failure
How to prevent Cystic Fibrosis?
Cystic Fibrosis can’t be prevented. Avoid marrying people with family history of Cystic Fibrosis. If parents have cystic fibrosis in their family, genetic testing can be done through amniocentesis (Remove fluid from the pregnant uterus) to rule out cystic fibrosis in the unborn baby. Genetic counselling before marriage is done to prevent producing babies with cystic fibrosis.
Cystic Fibrosis Causes, Signs, Symptoms and Treatment. Read More »
What is Epiglottitis ? Causes, diagnosis and treatment of epiglottitis

What is Epiglottis?
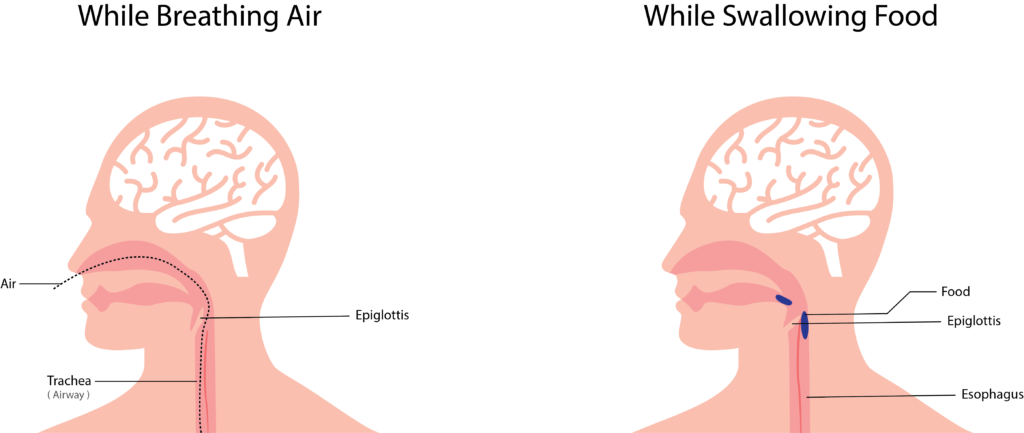
- Epiglottis is a leaf shaped soft bone (cartilage) at the base of the tongue.
- It is a flap like structure, which block the entry of food materials from entering the windpipe.
- Epiglottis open during movement of air in and out of respiratory organ and give way for air to enter the airway.
- It rolls backward while swallowing and prevent foreign particles that enter the airway and breathing organ [lung].
What is Epiglottitis?
Epiglottitis is the swelling (inflammation) of the epiglottis.
Enlargement of epiglottis may lead to blockage of upper airway by blocking the entry of air during respiration.
It usually causes breathlessness and blockage of windpipe. It is a medical emergency and may lead to death if proper treatment is not initiated immediately.
What are the causes of epiglottitis?
- Direct or indirect injury to epiglottis
- Intake of hot substance
- Inhalation of smoke, acid fumes and other irritants.
- Bacterial infection: Hib [haemophilus influenzae], Streptococcus pneumonia
- Fungal Infection: Candida,
- Viral Infection: Herpes simplex.
Who are infected often?
Epiglottitis usually affects children, but it can occur at any age. Epiglottitis affects non immunized and malnourished people.
What are the signs and symptoms of Epiglottitis?
- Fever (increase in body temperature)
- Hoarseness of voice
- Cough
- Painful swallowing
- Throat pain can occur with or without swallowing
- Stridor [musical breathing]
- Speaking difficulty
- Cyanosis (bluish coloration of face lips etc.)
What are the Four D s in epiglottitis?
Dyspnoea: difficulty in breathing,
Dysphagia: difficulty in swallowing,
Dysphonia: difficulty in speaking (voice disorder),
Drooling: dribbling of saliva.
How to diagnose epiglottitis?
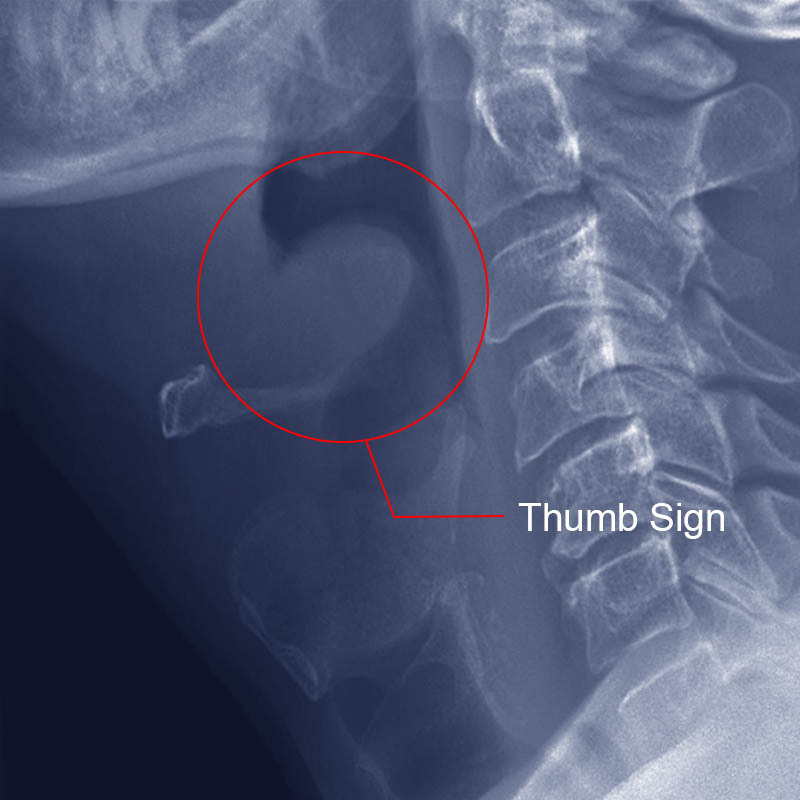
- Chest X-ray and lateral view of neck.
- Thumb sign- enlarged epiglottis will look like thumb in lateral view of neck.
- Throat swab for gram stain, culture and drug sensitivity testing.
- Routine Blood tests
- Laryngoscopy.
Treatment for epiglottitis
- Administration of oxygen (to maintain oxygenation)
- Endo tracheal intubation (to maintain an airway with artificial breathing support system)
- Antibiotics (stops the growth of bacteria and kills the cause of infectious organisms)
- IV fluids
- Position the patient [sit up-right position]
- Cool mist humidification
How can we prevent Epiglottitis?
- Avoid drinking very hot drinks.
- Avoid inhaling toxic fumes.
- Wash hands often and avoid placing fingers in to mouth and nose.
- Increase natural immunity with nutritious food.
- Vaccination: By taking Hi b ( Haemophilus influenzae –type B) Vaccinatin.
What is Epiglottitis ? Causes, diagnosis and treatment of epiglottitis Read More »
Endotracheal Intubation

What is Intubation?
Intubation ( Endotracheal Intubation ) is a process of placing a tube in the airway from the nose or mouth to trachea (wind pipe) to provide artificial respiration.
Who may need Intubation?
Intubation is done in patients with conditions such as respiratory failure, cardiac arrest, trauma etc.
Intubation is done in patients who cannot maintain a clear airway, who have severe airway obstruction and in patients who are unable to breathe on their own. It is also done to give general anesthesia and to start mechanical ventilation.
Intubation procedure must be carried out by well-trained medical professionals like doctors, respiratory therapists etc . Intubation is done in emergency conditions in ICU and operation rooms.
Equipments Needed
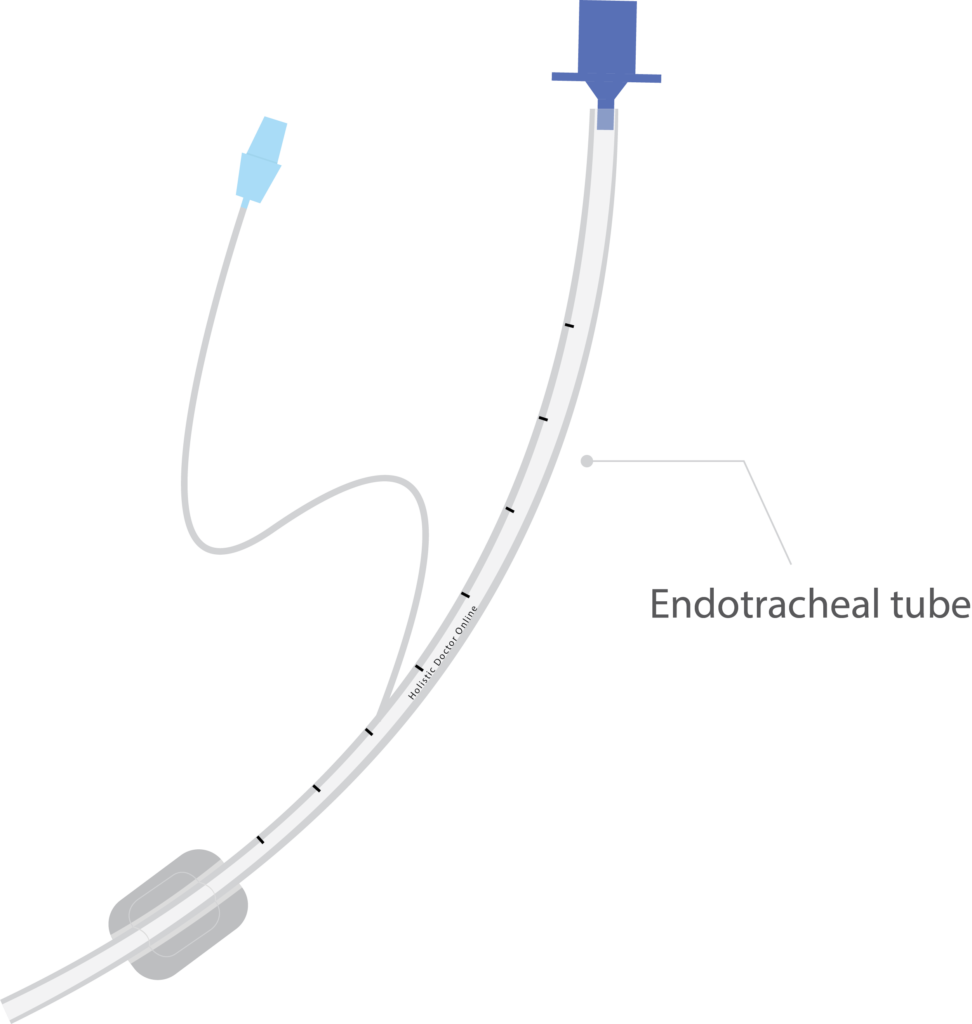
- Endotracheal tubes
- Laryngoscope with assorted blades
- Oxygen flowmeter and tubing
- Suction apparatus
- Flexible sterile suction catheters
- Sterile gloves
- Yankauer (tonsillar) tip suction
- Manual resuscitation bag and mask
- Colorimetric CO 2 detector
- Oropharyngeal airways
- PPE (gloves, gowns, masks, goggles or face shields)
- Laryngoscope with assorted blades
- Tongue depressor
- Stylet
- Stethoscope
- Tape or ET tube holder
- 10 or 20 ml syringe
- Water-soluble lubricating gel
- Magill forceps
- Local anesthetic spray
- Towels (for positioning the patients)

What preparation were done before intubation?
Before intubation the equipment’s must be checked and assembled. ET tube and laryngoscope must be selected according to patient’s size.
Before intubation ET tube must be checked for cuff leaks, it must be inflated and deflated with syringe. Bulb, blade, battery must be checked in the laryngoscope. Other equipment’s such as syringe tongue depressor, sty let, tapes, and Magill forceps must be checked and assembled.
Yankaeur suction can be used for oral suctioning. Vacuum pressure should be checked before suctioning. Suctioning is the process of applying negative pressure to remove the secretions and fluids in the airway. Before intubation patient should be 100% oxygenated with bag mask ventilation.
No intubation procedure must exceed 30 second. If intubation is not done within given with 30 second the oxygenation should be given with bag mask ventilation for 3 to 5 minutes.
In elective procedures, patients must be kept on fasting (no food or water) for a minimum period of 6 hours to prevent aspiration of food materials in to respiratory tract.
Premedication
For conscious patients sedation must be given to reduce anxiety. Patient is paralyzed to prevent resistance and to prevent vomiting. Local anesthetic is sprayed to numb the throat.
How intubation is done?
The medical professional doing intubation must stand behind the head of the patient. The patient must be in lying position. Sniffing position is done during the intubation; it is done by flexing the neck and tilting the head backward using hands. The sniffing position aligns patient’s mouth, pharynx and larynx in a same line and it opens the airway which helps in better visualization for the ET tube insertion.
The laryngoscope is an instrument which contains a holder and blade. It helps in better visualization of larynx. It consists of two types of blade – Miller (straight blade) and Macintosh (curve blade).
The medical professionals must use left hand to hold the laryngoscope and the right hand to open the mouth and to insert the tube. The laryngoscope must be inserted from the right side of the mouth; the tongue must be displaced to the left. The laryngoscope must be preceded until the visualization of epiglottis.
The epiglottis must be moved for the insertion of ET tube. Moving the epiglottis gives better visualization of vocal cord where the ET tube is inserted. Epiglottis is present at the entrance of voice box; this prevents the entry of food particles into the wind pipe. It opens during breathing, cough and sneezing etc.
The curve blade is positioned at the base of the tongue the laryngoscope is lifted up and forward for moving of epiglottis. The straight blade is positioned posterior to epiglottis were the laryngoscope is lifted up and forward for moving epiglottis. If the glottis is visualized the ET tube must be inserted from the right side of the mouth. The ET tube should be passed inside the airway until the cuff enters the vocal cords.
Stylet must be used for a stiff placement of ET tube. ET tube is passed easily if water soluble jelly is applied over the tube. Once the ET tube is inserted in the airway laryngoscope and stylet must be removed.
The cuff should be immediately inflated with a 10ml syringe. The cuff helps to maintain the tubes position in the wind pipe and also prevents the entry of foreign particles into the lungs. The ET tube must be placed 3 to 6 cm above the tracheal bifurcation (division of trachea).
Methods to check the position of endotracheal tube
Chest wall movements – After ET tube placement bag mask ventilation should be done. If bilateral chest wall movement is observed the ET tube is located above the carina. If abdominal bloating is observed, the ET tube is placed in the food pipe and re intubation should be done in this condition.
Bilateral lung sounds – Auscultation is done to check the bilateral lung sounds. If no lung sound isobserved in the left lung the ET tube is placed the right main bronchus. In this condition the ET tube must be slightly pulled out. If there is absence of lung sound the ET tube is in the food pipe. Reintubation should be carried out.
Bronchoscopy: This procedure shows the accurate position of the ET tube.
Capnometry: It is the measurement of CO 2 in the exhaled air. Normal PCO 2 in the exhaled air is 35 to 45mm of hg. If less amount of CO 2 is indicated the ET tube is in food pipe and re intubation should be done in this condition.
Chest x-ray: The radiograph line present in the ET tube shows the position of ET tube in the airway.
Tube length: The length marking present in the ET tube is used to determine the positioning. The tube length from the teeth to the tip is used to rule out the depth of the ET tube in the airway.
After confirmation of the ET tube placement in the airway it is held in position with tapes or tube holder. Oropharyngeal airways are placed to prevent the tongue fall back & to prevent the biting of tube. Then the ET tube is connected to the ventilator.
How to remove ET tube?
When the patient is weaned from mechanical ventilator and the patient cab breath on his own, ET tube can be removed. The adhesive tape holding the ET tube to the face is removed, the cuf of the Et tube is deflated and the ET tube is slowly pulled out.
What are the complications of Intubation?
Intubation can produce tissue damage, bleeding, improper placement leading to cerebral ischemia and brain damage. It can damage the larynx and vocal cord and produce speech problems. Intubation can also produce tracheal stenosis, tracheooesophageal fistula, pneumothorax, atelectasis and infection.
Endotracheal Intubation Read More »
Pneumonia: Symptoms, Causes, Treatment and Prevention
What is pneumonia?
Pneumonia is the inflammation of the lung parenchyma ( tissue that involves in gas exchange in the lungs otherwise called alveolar tissue ). When inflammation is caused by infection it is called pneumonia and when inflammation is caused by other causes like radiation, inhalation of chemicals etc… it is called as pneumonitis.
What are the causes of pneumonia?
Pneumonia can be caused by infection, inhalation of chemicals and gas or by aspiration of foreign bodies.
What happens to the lung in pneumonia? (Pathology)
- Stage of congestion
There is vascular engorgement and the intra-alveolar spaces are filled with fluid, blood cells and bacteria. - Stage of red hepatization
Exudates develops and the area is filled with pus and blood and the area becomes firm like liver. - Stage of grey hepatization
Slow disintegration of red cells and fibrin exudates forms. - Stage of Resolution
The thick exudates undergo enzymatic digestion. The debris are removed by macrophages and coughed out. It may heal fully of fibrosis occur.
What are the symptoms of pneumonia?
- Cough: Dry or Productive with sputum.
- Fever: with rigor (chills)
- Difficulty in breathing (shortness of breath)
- Fatigue
- Cyanosis (bluish coloration of tongue lips ect)
How Pneumonia is classified? – Types of pneumonia
Pneumonia can be classified according to
1. The anatomical site involved
- Eg: Bronchopneumonia, Lobar pneumonia.
2. The Source of infection
Community Acquired Pneumonia (CAP)
- Eg: Infection acquired from the society.
Hospital Acquired Pneumonia (HAP) – Nosocomial Pneumonia
- Pneumonia acquired from the hospital and manifesting after 48 hours after admission.

Ventilator Acquired Pneumonia (VAP)
- Appears 48 hours after starting mechanical ventilation.
Health Care Associated Pneumonia
- Pneumonia acquired from health care personals when the patient took out patients treatment or while undergoing procedures like dialysis, dressing, IV fluids etc…
3. The organisms causing
Bacterial
- Streptococcus pneumonia, Staphylococcus pneumonia.
Viral
- H1N1 pneumonia, COVID 19 Pneumonia.
Fungal
- Coccidioidomycosis
Chemical
- Infection after inhalation of gas or acid fumes.
Aspiration
- Infection after aspiration of stomach acid, water etc…
Investigation For Pneumonia
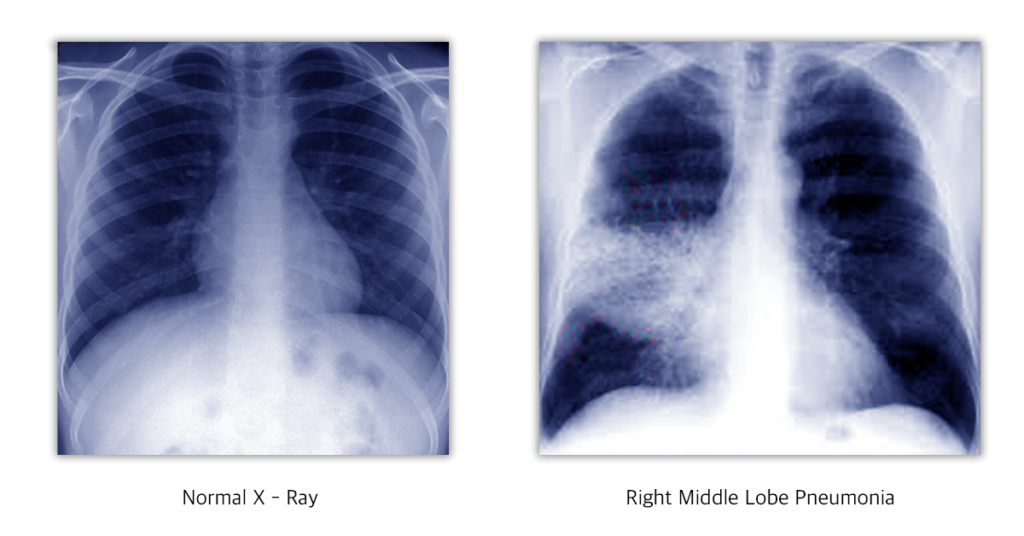
X-ray Cheat, HRCT Thorax, Sputum examination: Gram stain and AFB stain, Sputum culture and sensitivity, Blood culture, Serological tests for viral infection and to rule out HIV infection, Routine investigations like CBC, blood sugar, urea and creatinine.
How to assess the Prognosis?
Prognosis can be assessed using CURB-65 scoring system.
One point is given for each.
C – Confusion
U – Urea: more than 7 m mol/L
R – Respiratory rate: more than 30/ minute
B – Blood pressure: less than 90 systolic and/ or 60 diastolic.
65 – Age above 65.
Severity
If the total score is
0 to 1 – Mild outpatient treatment is enough.
2 – Hospital admission necessary.
3 to 5 – Severe, intensive treatment necessary, the death rate increases as the score.
Treatment For Pneumonia
Mild patients can be treated as outpatients with oral antibiotics and antipyretics. Moderate and severe patients need injections and intravenous fluids with oxygen support. Severe patients may need mechanical ventilation.
Broad spectrum antibiotics are started and later on altered according to the culture and sensitivity report.
Fever, body pain and other symptoms can be treated accordingly.
Prevention
Pneumococcal vaccine (like 23 valent pneumovax) can be given to vulnerable people like senior citizens over 65 years, diabetics, patients with pre existing lung disorders or patients on immunosuppressant drugs.
Pneumonia: Symptoms, Causes, Treatment and Prevention Read More »
Internet addiction
Article written by Ravindran O.S & Aruna Mani
Internet addiction
Internet addiction is characterized by excessive use of the internet, and that is detrimental to the user. There exists no clear definition for internet addiction as there is lot of uncertainty and disagreement among experts about overuse of the internet, the symptoms, how to measure it and even the language used to describe it as explained by the American Psychiatric Association. An American psychiatrist Jerald Block, (2008) stated that there exists three types of internet addiction: excessive gaming, sexual preoccupations, and email/text messaging, and all three types share four components: excessive use, withdrawal, tolerance for the costs of the activity and negative repercussions.
Different Types of Internet Addiction
A foremost expert on Internet Addiction Disorder, Young (2011) grouped internet addiction into six subtypes which are as follows:
- Internet Gaming
- Internet Gambling
- Internet Infidelity
- Internet Pornography/ Cyber sexual activities
- Information Overload
- Internet Compulsive buying
Personality Traits and Internet Addiction
Many research studies conducted in the past reveal the strong association between internet addiction and personality traits. Previous studies found a positive association between problematic internet use and interpersonal problems such as social skill deficiency, loneliness and social anxiety (Caplan, 2005, 2007., Morahan-Martin and Schumacher, 2000, 2003.,). Similar findings from another study revealed shy people or those disappointed by real relationships exhibit a certain behavior style which aims at finding a way to reach the outer world so that they are able to control it (Morrison and Gore, 2010). Impulsive behaviours (Reed et al, 2015), loneliness, alexithymia and suicide (Alpasla, et al, 2015) are also associated with excessive internet use. In young adults, social anxiety has been linked with internet addiction (Weinstein, et al, 2015), lower levels of family functioning, life satisfaction, and problems in family interactions (Wartberg, et al, 2015). It was also found to give rise to incidences of substance use, poor emotional well-being, and decreased academic performance in adolescents (Rucker, et al, 2015) and increased academic stress (Jun & Choi, 2015). People found to be higher in narcissistic personality traits tend to be more active on facebook and other social networking sites in order to present themselves favourably online because the virtual environments empowers them to construct their ideal selves (Buffardi & Campbell, 2008; Mehdizadeh, 2010).
Warning Signs for Internet Addiction
Diagnostic assessment of Internet Addiction Disorder proposed by Beard (2005) is widely accepted. He proposed five diagnostic criteria in the identification of Internet Addiction Disorder in the general population which are as follows:
- Is preoccupied with the Internet (constantly thinks about past use or future use)
- Needs to use Internet with increased amounts of time to gain satisfaction
- Has made unsuccessful efforts to control, cut back, or stop use of the Internet
- Is restless, moody, depressed, or irritable when attempting to control Internet use
- Has stayed online longer than originally intended
In addition, Beard suggested at least one of the following must be present in a diagnosis of Internet Addiction Disorder:
- Has jeopardized or risked the loss of a significant relationship, job, educational, or career opportunity because of the Internet
- Has lied to family members, therapists, or others to conceal their involvement with the Internet
- Uses the Internet as a way of escaping from problems or to relieve a dysphoric mood (e.g., guilt, anxiety, depression, helplessness).
Effect of Internet Addiction
Effects of internet addiction can manifest as physical or emotional. Some of the common emotional reactions are feelings of guilt, dishonesty, difficulty in keeping up with deadlines, poor time management, isolation, avoidance behavior, and agitation. Some of the physical effects manifested include headache, weight loss or gain, sleep disturbances, backaches, vision problems, and reduced self-care. Prolonged internet addiction has also been observed to have correlation with psychiatric and psychosocial conditions. Some of the commonly observed conditions are low self-esteem, impulsivity, poor sleep quality, mood disorders, suicide, ADHD, social phobia and depression, and in some cases even leading to loss of job, bankruptcy, and failed relationships.
Management
Internet addiction, though is not an official diagnosis in the Diagnostic Statistical Manual, however, it is believed to share similarities with impulse control disorders and gambling addiction. Treatment for internet addiction argued by some authors indicate that total abstinence from the internet should not be the goal of any intervention, and that instead an abstinence from problematic online activities and regulated use of the activity should be achieved (Cash H, et al. 2012, Khazaal Y, et al. 2012). However, more empirical evidence is needed to validate such claims. In terms of psychological treatment for internet addiction, cognitive-behavioral therapy is the most influential.
- Cognitive behavior therapy: In this model, the first stage of treatment is focussed on the behavioral aspects of the patient, so that at subsequent stages the focus of treatment is gradually shifted towards development of positive cognitive assumptions. During therapy, internet addicts identify false beliefs and learn how to modify them into more adaptive ones (Przepiorkal AM, 2014). Further, the therapy approach also promotes that patients should monitor their thoughts in order to identify affective and situational triggers associated with their addictive behavior (Khazaal Y, et al. 2012).
References
- Caplan, S. E. (2005). A social skill account of problematic Internet use. The Journal of Communication, 55(4), 4721-736. doi:10.1111/j.1460-2466.2005.tb03019.x
- Caplan, S. E. (2007). Relations among loneliness, social anxiety and problematic Internet use. Cyberpsychology & Behavior, 10, 234-242. doi:10.1089/cpb.2006.9963
- “Computer/Internet Addiction Symptoms, Causes and Effects” (2019). Retrieved from https://www.psychguides.com/behavioral-disorders/computer-internet-addiction/
- Gregory, C., (2019). Internet Addiction Disorder: Signs, symptoms, diagnosis, and treatments for those who may be addicted to the Web on their PC or smartphone https://www.psycom.net/iadcriteria.html
- Halley M Pontes, Daria J Kuss, Mark D Griffiths (2015). Clinical psychology of
Internet addiction: a review of its conceptualization, prevalence, neuronal processes, and implications for treatment. Neuroscience and Neuroeconomics. 2015. 4, 11-23. doi: https://doi.org/10.2147/NAN.S60982
- Kayis, A.R., Satici, S.A., Yilmaz, M.F., Simsek, D., Ceyhan, E., Bakioglu, F., (2016).
Big five-personality trait and internet addiction: A meta-analysis review. Computers
in Human Behavior
- Morahan-Martin, J., & Schumacher, P. (2000). Incidence and correlates of pathological Internet use among college students. Computers in Human Behavior, 16(1), 113-29. doi:10.1016/S0747-5632(99)00049-7
- Morahan-Martin, J., & Schumacher, P. (2003). Loneliness and social uses of the Internet. Computers in Human Behavior, 19(6), 6659-671. doi:10.1016/S0747-5632(03)00040-2
- Morrison, C. M., & Gore, H. (2010). The relationship between excessive Internet use and depression: A questionnaire-based study of 1,319 young people and adults. Psychopathology, 43(2), 2121-126. doi:10.1159/000277001
- Przepiorka AM, Blachnio A, Miziak B, Czuczwar SJ. Clinical approached to treatment of Internet addiction. Pharmacol Rep. 2014;66(2):187-191.
- “Virtual Addiction” David N. Greenfield, Ph.D., “Caught in the Net” Dr. Kimberly Young, Center for Internet Addiction Recovery, American Psychiatric Association.
- Young, K. (2011). Internet Addiction A Handbook and Guide to Evaluation and Treatment.
Internet addiction Read More »
Dark circle under the eye
Dark circle under the eye
Dark circle under the eye is one of the common cosmetic problems faced by both men and women. It may make them appear older and it gives them a hollowed –out look (ghost like look).
What causes the dark circles?
Dark circle under the eye can be caused by a combination of causes.
The causes are:
Over Exhaustion, Overstraining and tiredness can produce dark circle under the eye.
Physical Stress, mental stress, Sleep deprivation (Not getting enough sleep) and rubbing the eyes vigorously can produce dark circles under the eyes.
Dehydration (not drinking enough fluids) can also produce dark circles.
Ageing, genetic conditions and hormonal imbalance can cause dark circles under the eyes.
Anemia (Iron Deficiency), Vitamin Deficiencies, and malnutrition can cause dark circles under eyes.
Allergies and skin diseases can also produce dark circles.
Over exposure to sunlight, Using inappropriate eye glasses, refractive errors of the eye and overstrain of the eye (like using computers or mobile phones for long without rest) can cause dark circles under the eyes.
How to get rid of dark circles under the eyes
General Treatment:
Good rest to the eyes. Eight hours of sleep, Reduction of stress, Eating a well balanced diet with lots of green leafy vegetables and fruits and Drinking lots of fluids can prevent and reduce dark circles under the eyes.
Natural Cure for dark circles under the eyes:
LEMON JUICE: Applying lemon juice over the dark circles and washing it off with cool water after 20 minutes can reduce dark circles.
CUCUMBER: Keeping slices of cool cucumber over the eyes and taking rest for 20 minutes or applying cucumber juice over the dark circles and washing it off after 20 minutes reduces dark circles under the eyes.
POTATOES: Cool potato slices kept over the eyes or applying cool potato juice over the dark circles and washing it off after 15 to 20 minutes helps to reduce dark circles under the eyes.
Applying a mixture of lemon juice, potato juice and cucumber juice over the dark circles and washing it off after 20 minutes gives better and faster results.
MILK: Milk moisturizes and lightens the skin. Applying cotton pads soaked in cold milk over the dark circles and washing it off after 30 minutes gives good results.
GREEN TEA: Refrigerated & soaked green tea bags can be kept over the eyes for15 minutes to reduce dark circles.
Tomato juice, Coconut oil, Honey, Almond oil, Vitamin E, Turmeric powder, mint, licorice extract or baking soda can be applied over the dark circles and washed after 15 to 20 minutes can reduce dark circles under the eyes.
Other Treatments Available:
LASER THERAPY: Sending burst of laser light to Dark circles may tighten the skin and allow growing new lighter skin.
CHEMICAL PEELS: Chemical peels using Retinoic acid or Hydroquinone help to reduce dark circles.
Intense Pulse Light Therapy (ILP) and Plastic surgery can also be used to treat dark circles under the eyes.
The dark circles can be camouflaged or concealed with makeup.
How to prevent dark circles under the eyes?
To prevent dark circles under the eyes take nutritious well balanced diet.
Avid smoking, excessive alcohol, and late night parties. Look away from computer or mobile screen every few minutes. Have minimum 8 hours of good sleep.
Avoid over exposure to sun light. Use sun screen when going out in hot sun. Use dark sunglasses prescribed by doctors.
Drink lot of fluids like fruit juices and tender coconut water when going out in hot sun to prevent dehydration.
Dark circle under the eye Read More »