What is Tracheal Extubation?
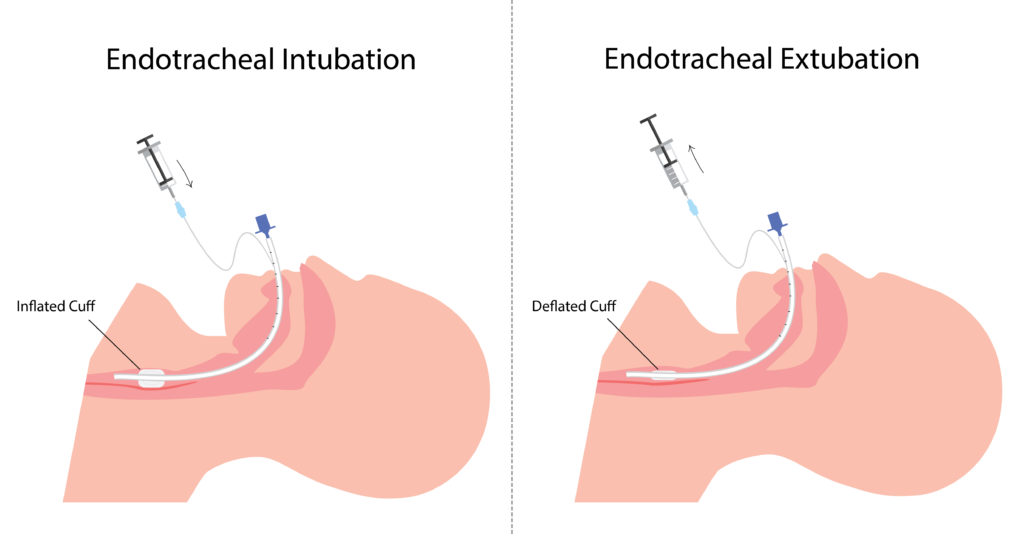
Endotracheal tube is a flexible polyvinyl chloride tube which helps to assist breathing. The process of placing endotracheal tube in the airway is called Intubation. Intubation is done to provide artificial breathing. Tracheal extubation is the process of removing the endotracheal tube from the airway.Extubation is done, once the patient is weaned (gradual withdrawal) from the ventilator.
What are the indications for Tracheal Extubation?
When the patient has improved and no longer need artificial airway to breathe. If the patient is maintaining adequate gas exchange, perfusion and have improved breathing pattern and cardiovascular status.
If the patient is having improved airway protective mechanism such as cough to clear the secretions. The need for exchange of ET tube due to mucus and other secretion obstruction.
What are the contraindications for Tracheal Extubation?
In patients who cannot maintain clear airway.
In patients who have weak respiratory muscles, inadequateventilation and perfusion.
In patients who have persistent hypoxia and hypercarbia.
In patients who have severe cardiac instability, hypothermia andmetabolic imbalance.
What are the criteria for Tracheal extubation?
Before Extubation, Spontaneous Breathing Trial (SBT) is done to assess the capability of the patient to breathe in a minimum ventilatory support and oxygen support. In SBT, patient should complete 30 to 120 minutes with low level of Continuous positive airway pressure (CPAP) pressure support, showing normal breathing pattern, cardiovascular status and gas exchange.
Subjective assessment for Extubation
Adequate cough.
No neuromuscular blockers and sedatives.
Absence of excessive and thick secretions.
Improvement in disease condition.
Objective measurement for Extubation
Stable cardiovascular status.
Heart rate≤ 140 b/min.
No active myocardial ischemia.
Adequate hemoglobin levels ( ≥ 8g /dl).
Systolic blood pressure 90-160 mmhg.
Afebrile.
No or minimal vasopressor or inotrope.
Oxygenation assessment for Extubation
Tidal volume > 5ml / kg.
Vital capacity 10ml / kg.
Proper inspiratory effort.
Respiratory rate≤35minutes.
Rapid shallow breathing index<105.
PaO 2 ≥60 and PaCO 2 ≤60 mmhg.
PEEP ≤ 8cm h2O.
No significant respiratory acidosis ( PH ≤ 7.30).
Maximal inspiratory pressure (MIP) ≤‐20 – – 25 cmh2O.
O 2 saturation > 90% on FiO 2 ≤ 0.4.
What is Cuff Leak Test?
Cuff leak test is done before Extubation to check the presence of laryngeal edema which is one of the major causes of respiratory failure which leads to reintubation.
Test procedure for cuff leak test
The cuff is completely deflated with a 10ml syringe and tidal volume is measured.
Cuff leak calculation ;
Tidal volume before deflation- Tidal volume after deflation= cuff leak
The percentage of cuff leak should be 15%
It low cuff leak is detected the patient has edema.
Intravenous or nebulized corticosteroids and epinephrine are administered to treat the above conditions.
What are the equipments needed for Tracheal extubation?
All the equipments needed for the intubation must be checked and arranged, because in some cases reintubation may be required or respiratory failure may occur.
Important equipments for Extubation
Suctioning equipment
Scissors
10ml syringe
Bag valve mask resuscitator
Supplemental O 2
O 2 mask or NIV according to patients need
Crash cart
What is the procedure for Tracheal Extubation?
- Complete suctioning of upper airway and ET tube to prevent the entry of secretions in to the lower airway.
- The patient should be bagged with 100 % oxygen.
- The cuff is completely deflated using a syringe
- Remove the ET tube holder or tapes.
- Remove the ET tube;
A large breathe was given through the bag valve mask resuscitator, the tube is removed during maximal inspiration where the vocal cords are in open position.
The patient is encouraged to cough; the tube is removed at the expulsive expiratory phase where the vocal cords are in maximal open stage. - Oxygen therapy or NIV is provided according to the patient’s need.
- Auscultation is done to assess the presence of stridor or decreased air entry.
- The patient’s ABG values are checked. Heart rate, blood pressure, saturation should be continuously monitored.
What are the complications of Tracheal Extubation?
Common complications:
Hoarseness of voice
Sore throat
Cough
Other complications are,
Hypoventilation
Increased work of breathing
Respiratory muscle weakness
Aspiration due to improper suctioning
Pulmonary edema
Bronchospasm
Atelectasis
Laryngospasm
These complications of Extubation may lead to extubation failure.
What is Extubation failure?
When re-intubation is necessary within 24-48 hours of planned Extubation then it is called Extubation failure.
Non invasive ventilation (NIV) helps to reduce the chances of Extubation failure.
