What is Respiratory Distress Syndrome (RDS) in Neonates?
RDS once called Hyaline Membrane Disease (HMD) or Surfactant deficiency syndrome (SDD) is mainly seen in premature babies and manifest within few hours of birth due to surfactant deficiency and immature lungs. May cause death due to respiratory distress or insufficiency, if not treated on time.
What are the causes of Respiratory Distress Syndrome?
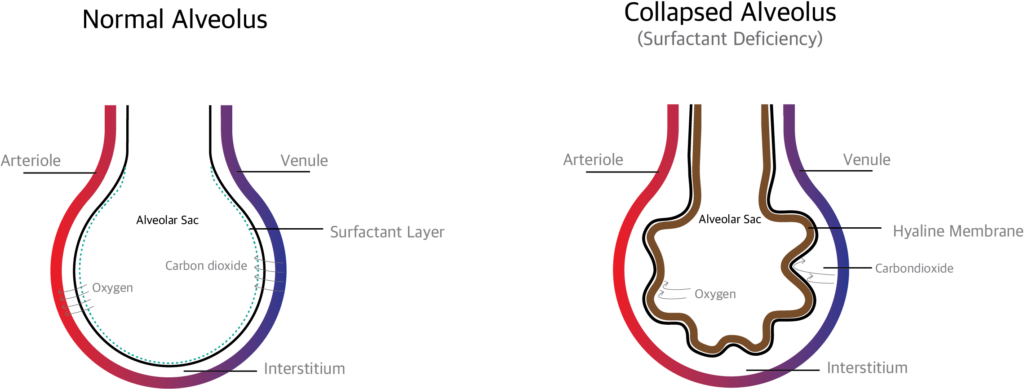
The main causes are immature development of the lung and inadequate surfactant (adequate surfactant, prevents collapse of the alveoli by reducing the surface tension of the fluid lining of the alveoli).
What are the most common contributing factors?
- Early birth (born before 7 months of pregnancy)
- When the mother has Diabetes mellitus
- When the newborn is born through Cesarean section delivery
- The previous sibling had RDS
- Hypothermia of the newborn
Pathophysiology of RDS
The surfactant production starts by 24 weeks of pregnancy. In case the baby is born before this period, there is a higher chance of surfactant deficiency which leads to respiratory distress.
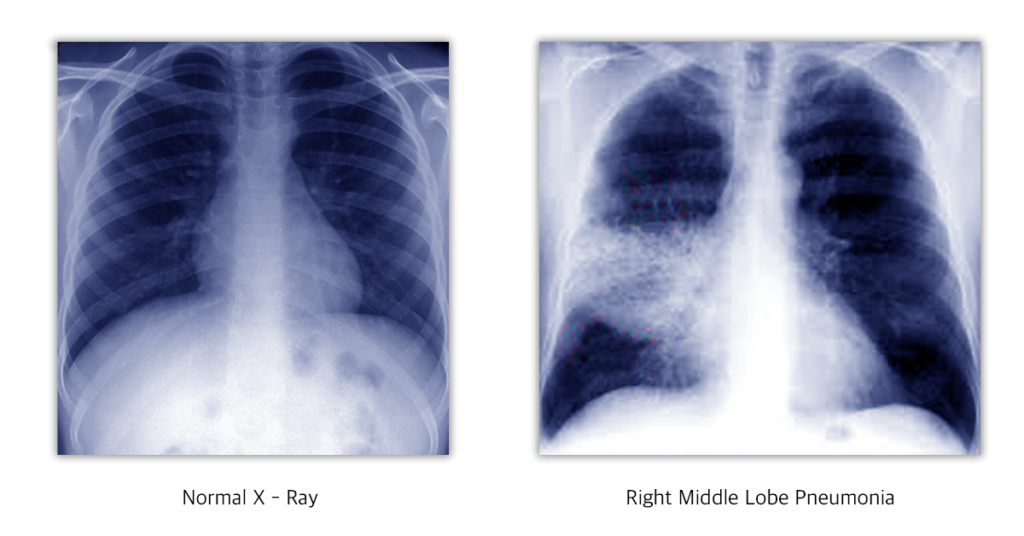
Normally when the baby is in mother’s uterus, the alveoli in the lung are filled with fluid. When the baby is born, the sudden change in environment and drop in temperature make the baby to take a deep breath. The fluid in the lung is reabsorbed and replaced with air.
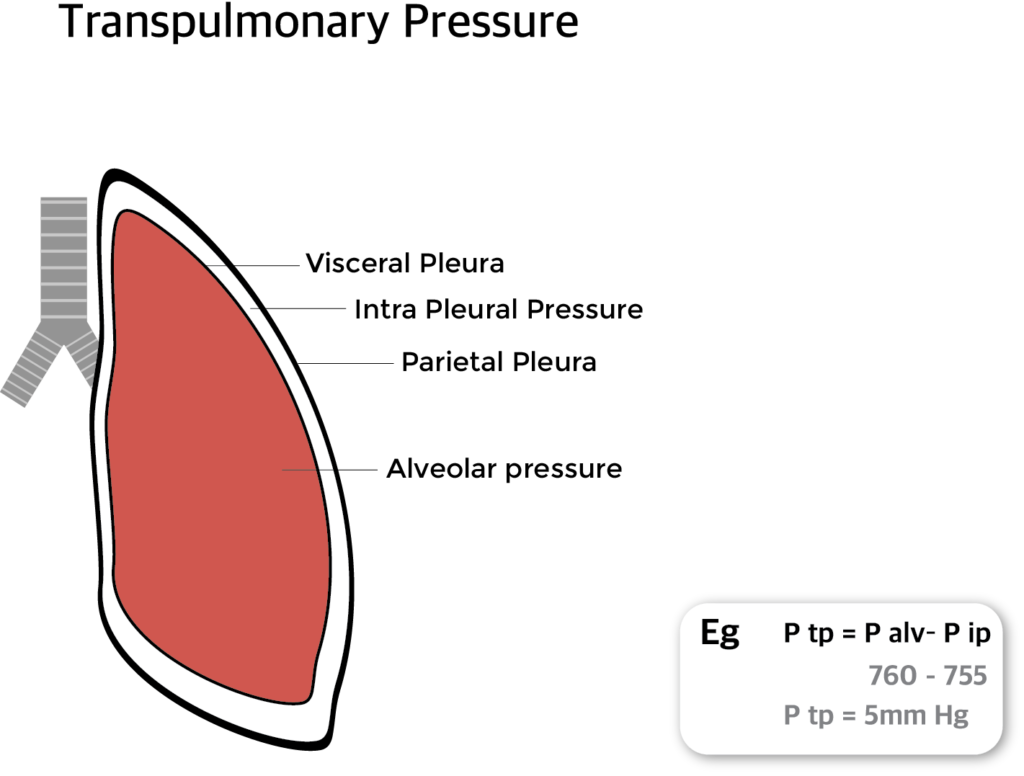
During expiration, the alveoli is prevented from collapsing by the surfactants.. If surfactant is deficient, the alveoli collapse which in turn produces hypoxemia, CO2 retention, etc.
When the alveoli collapse the damaged cells (alveolar cells, red blood cells, white blood cells and macrophages) collect and form a membrane like structure called Hyaline membrane which prevents gas exchange.
How RDS is diagnosed?
Diagnosis can be done either prenatally (before birth) or postnatally (after birth)
Prenatal (before birth): amniotic fluid index like Surfactant / albumin ratio, Lecithin / sphingomyelin ratio and presence of phosphatidyl glycerol (PG).in amniotic fluid.
Postnatal (after birth): through clinical signs and diagnostic tests.
What are the clinical signs of Respiratory Distress Syndrome?
- Increased respiratory rate
- Expiratory grunting (sounds like baby crying)
- Retraction (pulling inward of respiratory muscles) substernal, suprasternal and xiphoid
- Nasal flaring (widening of nostrils)
- Bluish discoloration (cyanosis)
What investigations (diagnostic tests) are done to diagnose RDS?
Oxygen saturation, Arterial blood gas analysis (ABG), routine blood investigations and blood sugar were done. X ray chest, echocardiogram and MRI chest can be done.
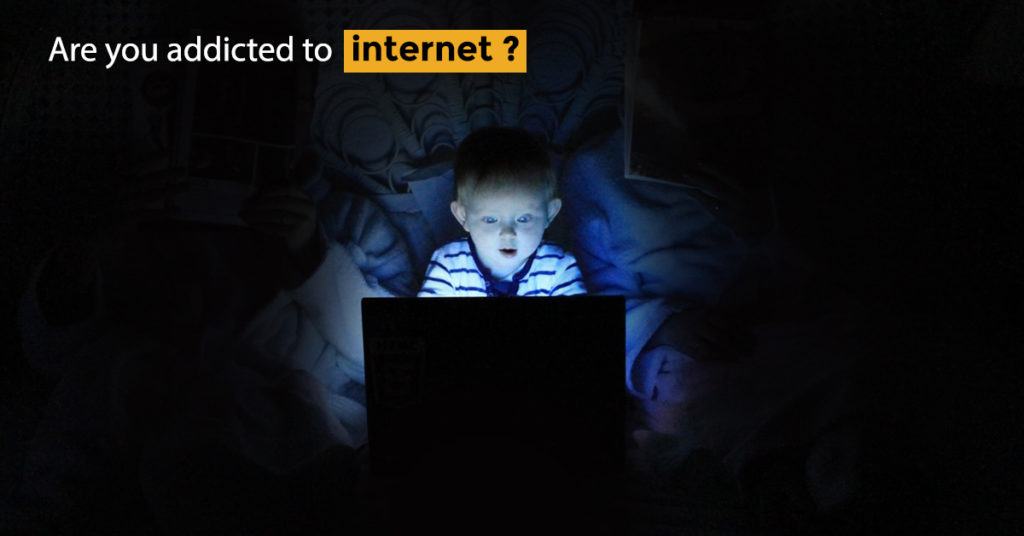
X ray findings in Respiratory Distress syndrome
X ray chest shows bell shaped chest, reduced lung volume and air bronchogram Staging
- Stage 1- infiltrates
- Stage2 – infiltrates with reticulogranular pattern
- Stage3- reticulogranular pattern extended and blurring the cardiac shadow
- Stage4- ground-glass opacity
What is the treatment (management) for Respiratory Distress Syndrome?
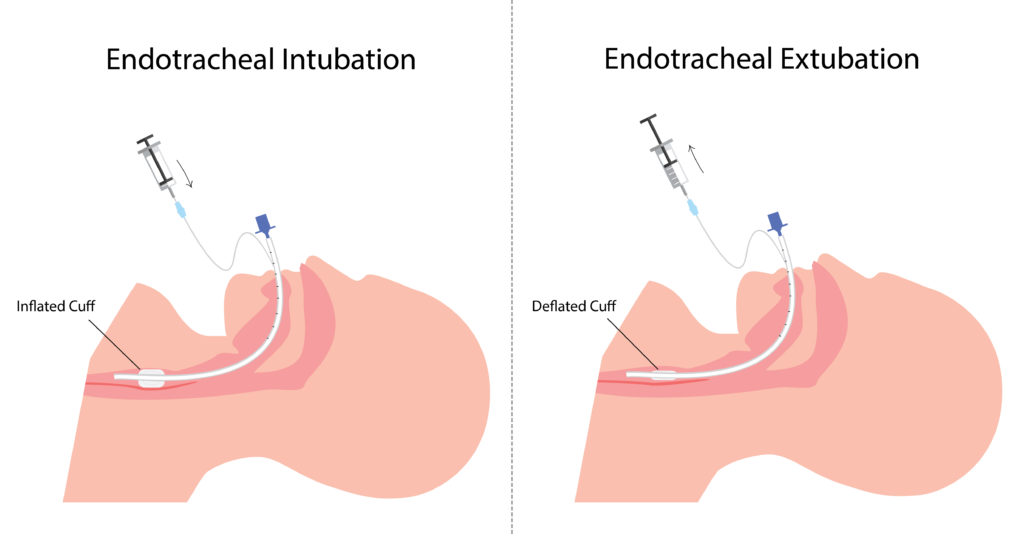
Start oxygen therapy and if necessary, support respiration with noninvasive ventilation like CPAP or intubate the baby and start mechanical ventilation.
Surfactant replacement therapy: Animal derived (bovine) or synthetic surfactant can be administered through endotracheal tube. Early CPAP and surfactant administration may reduce death rate (mortality), air leak and other complications. This can be continued till the baby produces enough surfactant.
Plan of care
Supportive management includes maintaining normal body temperature, adequate fluid, acid-base balance, and proper nutrition
Prevent infections by proper vaccinations.
What are the complications of RDS?
- Pneumothorax
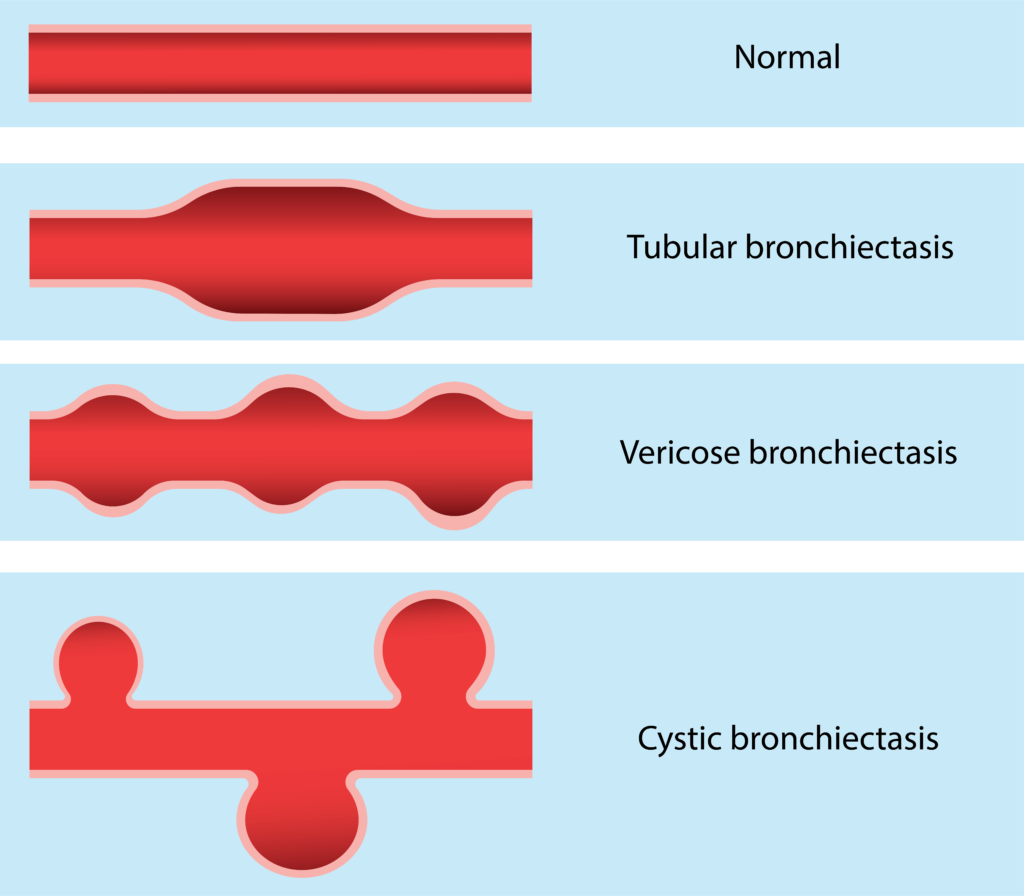
- Broncho Pulmonary Dysphagia
- Pulmonary hemorrhage
- Intra Ventricular Hemorrhage